Neonatology
Session: Neonatal Quality Improvement 2
398 - Improving Documentation of Communication with Families in the NICU
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 398
Publication Number: 398.2194
Publication Number: 398.2194

Danielle Garza, BS (she/her/hers)
Medical Student
University of Texas Medical Branch John Sealy School of Medicine
Galveston, Texas, United States
Presenting Author(s)
Background: Effective communication with families is essential in the Neonatal Intensive Care Unit (NICU), as research has shown significant impact on parental mental health. Parents of admitted babies have voiced their appreciation for timely and accurate updates during hospitalization. Documentation of these conversations is essential. Optimizing the electronic medical record (EMR) can help providers improve documentation without adding unnecessary burden. We created an EMR “smartphrase” that allows providers to document using a standardized template and monitored usage and authorship.
Objective: Improve documentation by 72 hours of life (HOL) and during hospitalization of family updates using a standardized template by 20% from baseline for all NICU admissions and assess usage and authorship of documentation from July 2022-2023.
Design/Methods: We created a standardized EMR smartphrase titled “Family Communication” for providers to use for all admissions to our Level IV NICU. The smartphrase launched in 7/2021 included who was updated, content of discussion, and whether a translator was utilized. After 1 year of use, we decided to expand the project and utilize new PDSA cycles to improve documentation and from July 2022-2023 at 72HOL and during hospitalization.
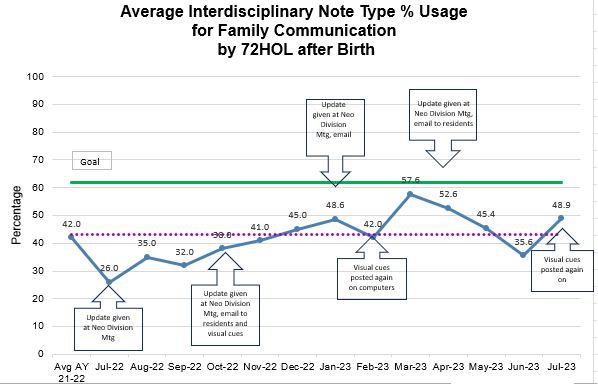
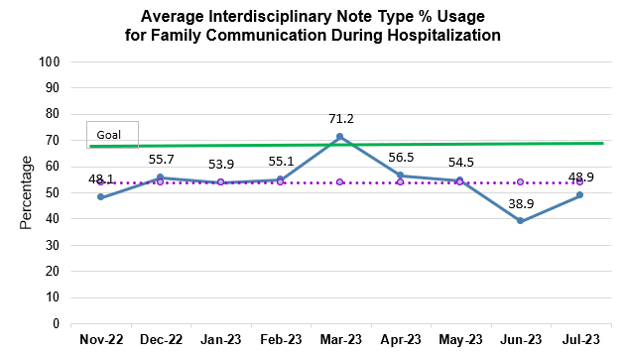
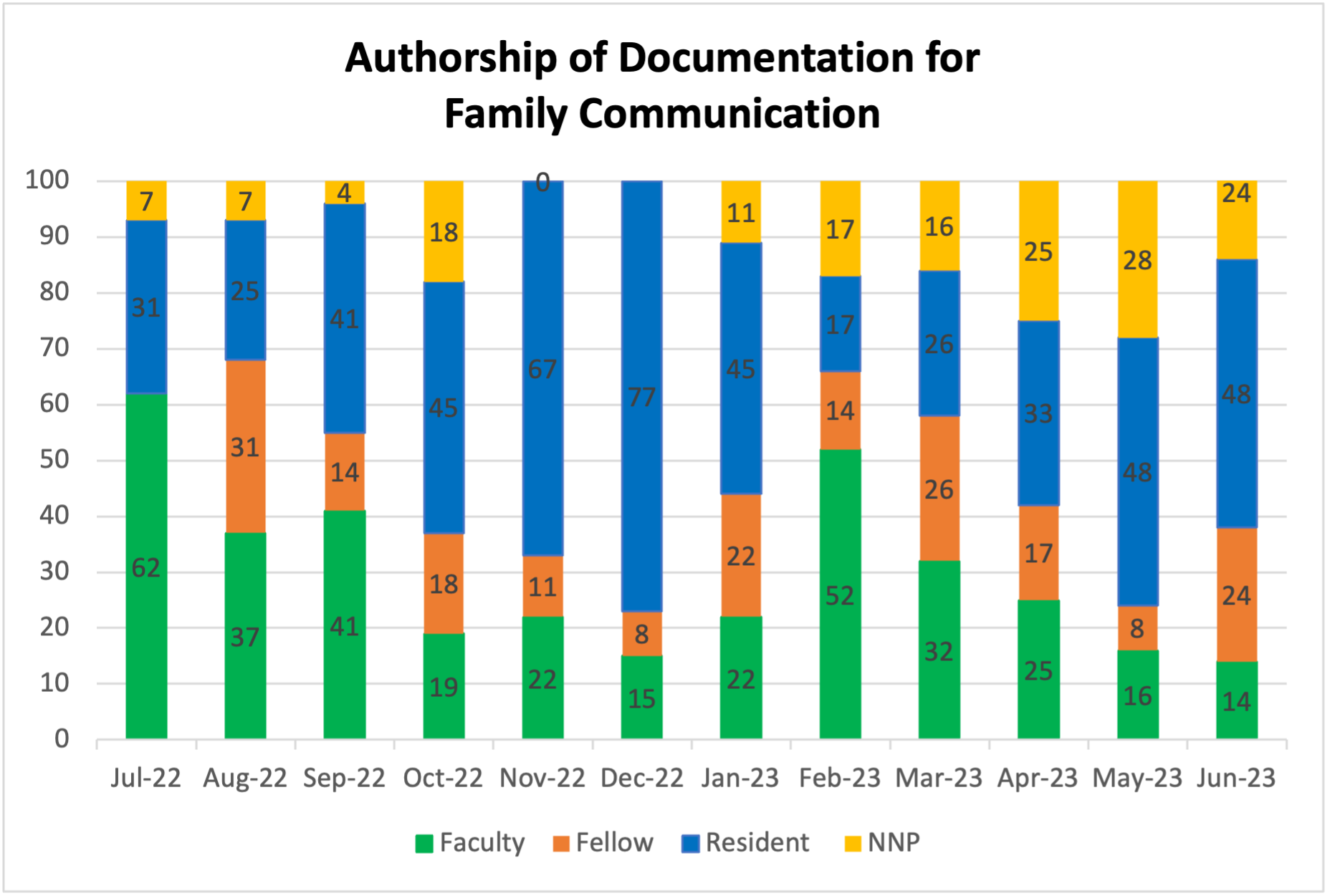
Results: Since implementation, providers have fluctuated in their documentation rate with decreases during periods of high acuity as well as near the start of a new academic year. On average, providers documented conversations within 72 HOL, 42% of the time with a steady increase since 7/2022 (Fig 1). Throughout hospitalization, providers documented 53.6% of the time (Fig 2). The most effective PSDA cycle interventions have been emailing reminders during trainee rotation switches and visual cues at workstations. Residents and fellows represent the majority in documentation, yet authorship patterns demonstrate that sustainability requires support from all levels of providers (Fig 3). Although we have not yet reached our goal, there is up trending and consistent documentation, and we continue to explore ways to make these family conversations a top priority.
Conclusion(s): The optimization of the EMR allows for timely and accurate documentation of conversations with families, an integral component of the care provided in the NICU. Visual cues and email reminders improved timely documentation over the course of a year. Trainees represent the majority of providers who have initial contact with the families and further research regarding the direct impact of these conversations with families is ongoing.