Neonatology
Session: Neonatal Follow-up 3
532 - Cognitive Outcomes of Neonates with Hypoxic-Ischemic Encephalopathy Treated with Hypothermia: The Impact of Socioeconomic Vulnerability
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 532
Publication Number: 532.2815
Publication Number: 532.2815

Srishti Jayakumar, MD, MPH (she/her/hers)
Fellow, Neonatal-Perinatal Medicine
Johns Hopkins University School of Medicine
Baltimore, Maryland, United States
Presenting Author(s)
Background: The role of maternal and neonatal factors in neurodevelopmental outcomes of infants surviving hypoxic-ischemic encephalopathy (HIE) treated with therapeutic hypothermia (TH) is established. However, there is limited literature examining how sociodemographic factors affect neurodevelopmental outcomes in these neonates.
Objective: Our aim was to elucidate the relationship between county-level socioeconomic vulnerability and cognitive outcomes of neonates surviving HIE.
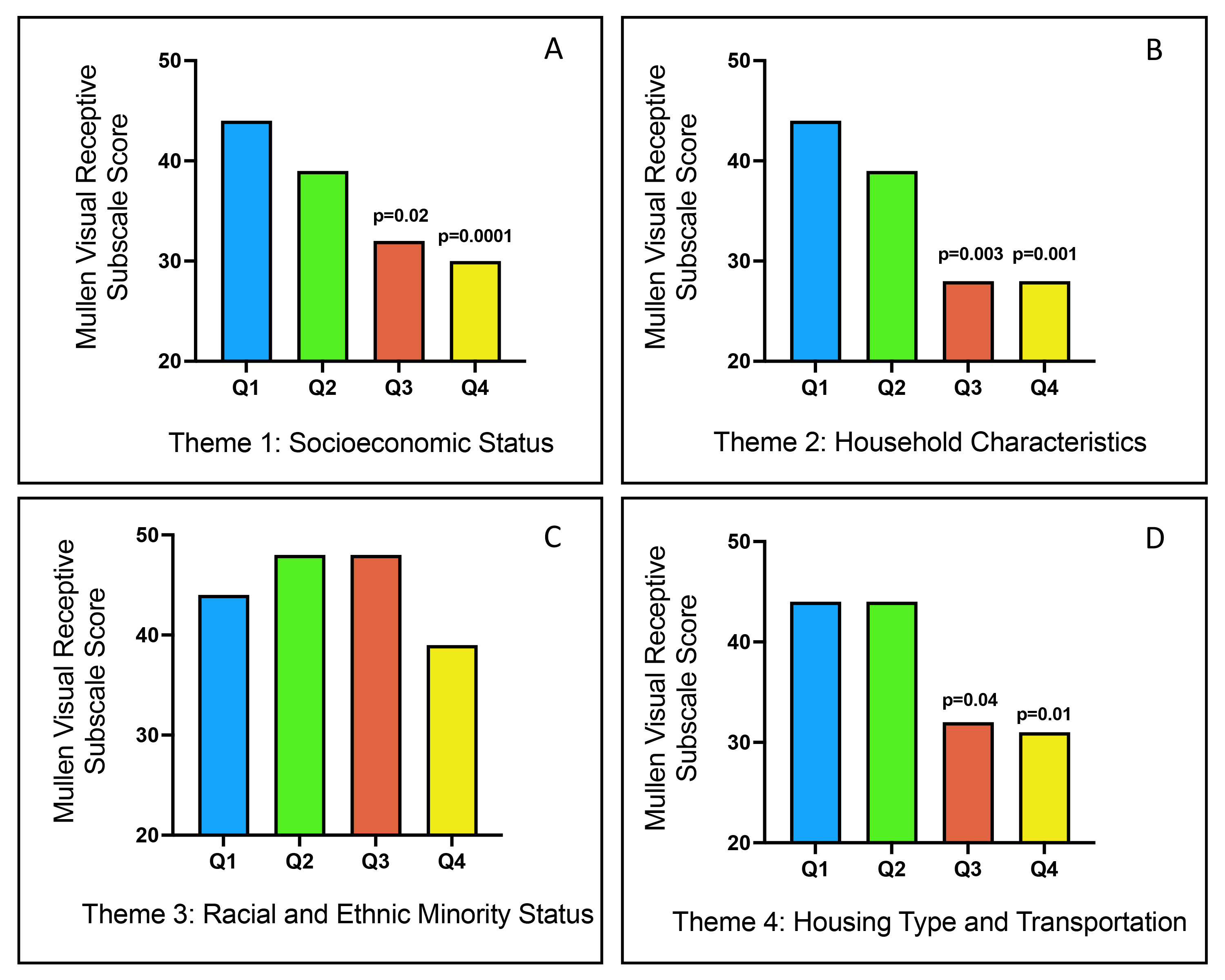
Design/Methods: 43 infants with moderate to severe HIE who underwent TH were enrolled between 2010 and 2015. Using electronic medical records, we obtained clinical and sociodemographic characteristics including birth anthropometrics, gestational age, sex, cord pH, base deficit, Apgar scores at 1 and 5 minutes, brain MRI NICHD scores, peak creatinine and alanine transaminase levels in the first 24 hours. We used the CDC Social Vulnerability Index (SVI), a well-validated metric comprising four themes based on 16 US Census indicators to assess vulnerability for the infant’s county of residence. We used Mullen scores comprising four subscales to assess cognitive and motor outcomes at 24 months. Regression analyses were performed to assess differences in outcomes in Mullen subscales by SVI quartiles adjusted for MRI NICHD scores.
Results: Among infants with HIE treated with TH, we observed significant MRI NICHD score-adjusted associations for county-level exposures including socioeconomic status (p = 0.04), household characteristics (p = 0.01), and housing type and transportation (p=0.01) with Mullen Visual Reception scores at 24 months (Figure 1). Similarly, we observed significant adjusted associations for socioeconomic status (p = 0.005), household characteristics (p = 0.007), and housing type and transportation (p=0.01) with Expressive Language scores at 24 months. While this association persisted between Fine Motor scores and each SVI theme, Receptive Language scores were preserved. Within each theme and across all components of the Mullen, infants from areas with higher SVI had significantly lower Mullen scores than infants from areas with less disadvantage.
Conclusion(s): All themes of county-level social vulnerability have a detrimental impact on all components of neurodevelopmental outcomes of children with a history of neonatal HIE. Further research elucidating the specific contributions of these individual components will allow for identification of populations most at risk. This will aid the development of evidence-based, targeted interventions to improve outcomes and the realization of each child’s full potential.