General Pediatrics
Session: General Pediatrics 4
360 - FosteRx: Empowering Foster Families with Comprehensive Health Information
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 360
Publication Number: 360.1258
Publication Number: 360.1258

Ashley M. Bach, MD MPH (she/her/hers)
Pediatric Neurology Resident
Childrens Hospital of Philadelphia
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: Children in foster care have high rates of chronic medical and behavioral health conditions, with nearly 90% requiring referral to ≥1 specialist and 25% requiring ≥3 specialists. Transitions between foster homes increase their risk of experiencing fragmented medical care, which may lead to missed preventative health services and disrupt follow-up with providers. Key health information has been noted to be at particularly high risk of loss during the transition to a new foster home.
Objective: To assess the implementation of an intervention to minimize loss of key health information for children in foster care. The intervention consisted of providing foster caregivers with a portable repository of health information and executing an electronic medical record (EMR) checklist.
Design/Methods: We conducted a pilot study to assess the implementation of a transition-of-care bundle for foster youth. Foster caregivers were provided with a customizable binder containing comprehensive medical information about their child, designed to be updated by the caregiver as needed (Table 1). Care packages with age-appropriate supplies were additionally provided to children entering a new home (Table 1). EMR checklists were implemented that prompted clinicians to update charts with children’s current caregiver contacts (Table 2). We assessed implementation outcomes of adoption, penetration, acceptability, feasibility, and fidelity. Qualitative feedback was collected from stakeholders including foster caregivers, DHS workers, and clinicians via anonymous semi-structured surveys distributed by QR codes. EMR checklist fidelity was assessed by chart review of a subset of children for whom identifiable information was available.
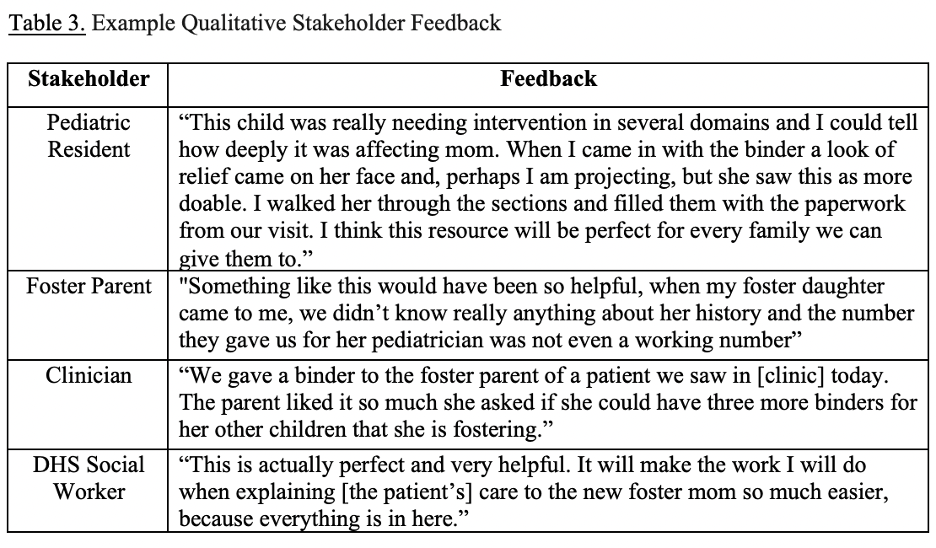
Results: Over 2 years, we served 120 children –17 inpatients and 103 outpatients – on 9 of 12 resident-staffed inpatient services, 2 of 2 trauma and rehabilitation inpatient services, 3 of 3 resident primary care clinics, and 2 clinics tailored to children in foster care, supporting adoption and penetration of the intervention. Qualitative feedback suggested that the intervention was well-received by stakeholders, who emphasized the utility of collating the information in one portable source (Table 3). Of 49 patient charts reviewed, 47 (96%) contained updated contact information for the foster caregiver.
Conclusion(s): Distribution of binders with comprehensive medical information for foster youth and EMR checklist implementation were feasible in inpatient and outpatient settings and well-received by stakeholders.
.png)
.png)