Neonatology
Session: Neonatal Quality Improvement 2
400 - Improving Skin to Skin for Late Preterm Infants.
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 400
Publication Number: 400.1961
Publication Number: 400.1961

Olubusayo M. Akinyemi, M.D (she/her/hers)
Fellow
Cohen Children's Medical Center
Glen Oaks, New York, United States
Presenting Author(s)
Background: Early skin-to-skin contact (SSC) between mothers and their newborn infants is an evidence-based best practice. Separating infants from their mothers increases the incidence of hypoglycemia, hypothermia and breastfeeding failure in the perinatal period, resulting in stress and elevated cortisol levels. However, the baseline rate of SSC among well 35- and 36-week gestation infants in our Mother-Baby Unit in January 2022 was only 62%.
Objective: Our SMART aim was to improve the rate of SSC among well 35- and 36-week gestation late preterm newborns in our Mother-Baby Unit to > 75% by 12/31/22. SSC was defined as any sessions documented by Nursing during the newborn hospitalization. Secondary outcome aims were to increase the rate of breastfeeding and decrease the rates of hypothermia ( < 36.5C) and hypoglycemia ( < 45 mg/dL point-of-care glucose) during that period.
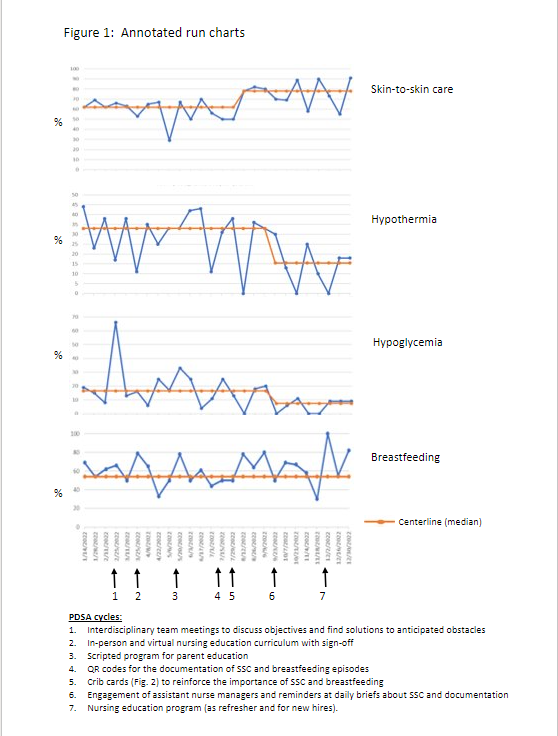
Design/Methods: Multiple interventions were implemented and evaluated by a multidisciplinary committee (see annotated run charts, Fig. 1). Temperatures were monitored frequently in the first 4 hrs and then every 4 hrs after birth. Point-of-care glucose was assessed hourly for the first 4 hrs, at 12 hrs, and at 24 hrs per clinical protocol. Data on SSC episodes, breastfeeding, temperature, and glucose were obtained from the EMR and frequencies calculated over 2 week periods.
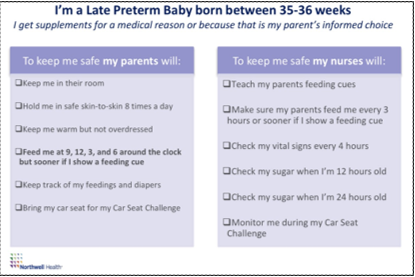
Results: The rate of SSC increased to 78% after the introduction of late preterm crib cards (Fig. 2) as visual prompts and QR codes to facilitate documentation. The rates of hypothermia and hypoglycemia declined to 15% (from 33%) and 7% (from 16%), respectively, after nursing leadership was actively engaged to discuss STS care with each nursing shift. Improvements were sustained by another structured education program for Nursing. However, the rate of breastfeeding did not change.
Conclusion(s): SSC care for late preterm infants increased only after the introduction of crib cards. This suggests that even when knowledge and intentions among staff and parents are good, implementation of SSC for these infants requires tangible instructions and prompts. The use of QR codes may have also contributed to increased rates of SSC by improving the documentation of sessions. We anticipate that this technology will enable us to better identify and target women at highest risk for failure in ongoing projects to improve the frequency and quality of SSC for late preterm infants. Announcements by nursing leadership at briefs for each shift may have reinforced multiple care pathways in addition to SSC, contributing to sustained decreases in hypothermia and hypoglycemia.