Children with Chronic Conditions
Session: Children with Chronic Conditions 1
257 - Children with Medical and Social Complexity: Caregiver Perspectives on Navigating the Healthcare, Education and Social Services Systems of Care
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 257
Publication Number: 257.336
Publication Number: 257.336

Jennifer B. Peralta, MD, MSHPM, MS (she/her/hers)
Health Sciences Clinical Instructor
University of California, Los Angeles
Los Angeles, California, United States
Presenting Author(s)
Background: Children with medical complexity (CMC) face unique care coordination challenges that span healthcare, education and social services systems. These navigation challenges may be exacerbated by social complexity (individual, family or community characteristics that affect a child's access to care and/or a family’s ability to engage needed care, i.e. multiple complex unmet social needs). However, less is known about how social complexity impacts care navigation, health and wellness for CMC and their caregivers, as well as how to best support CMC families with social complexity (CMC+SC).
Objective: To characterize CMC+SC caregiver perspectives on 1) how social complexity impacts their ability to navigate systems of care and support their child’s health and 2) to identify ideal characteristics of family-serving systems of care (healthcare, education and social services systems).
Design/Methods: Semi-structured interviews were conducted with 27 caregivers (21 English-speaking, 6 Spanish-speaking) with varying degrees of social complexity were recruited from 2 geographically distinct pediatric complex care programs (16 West Coast, 9 Midwest). Interviews were audio recorded and transcribed. Independent coding was performed, followed by transcript review and discussion of initial codes using a Constructivist Grounded Theory approach. Codes were refined through iterative analysis until thematic saturation was reached. A demographic and social needs screener was also administered.
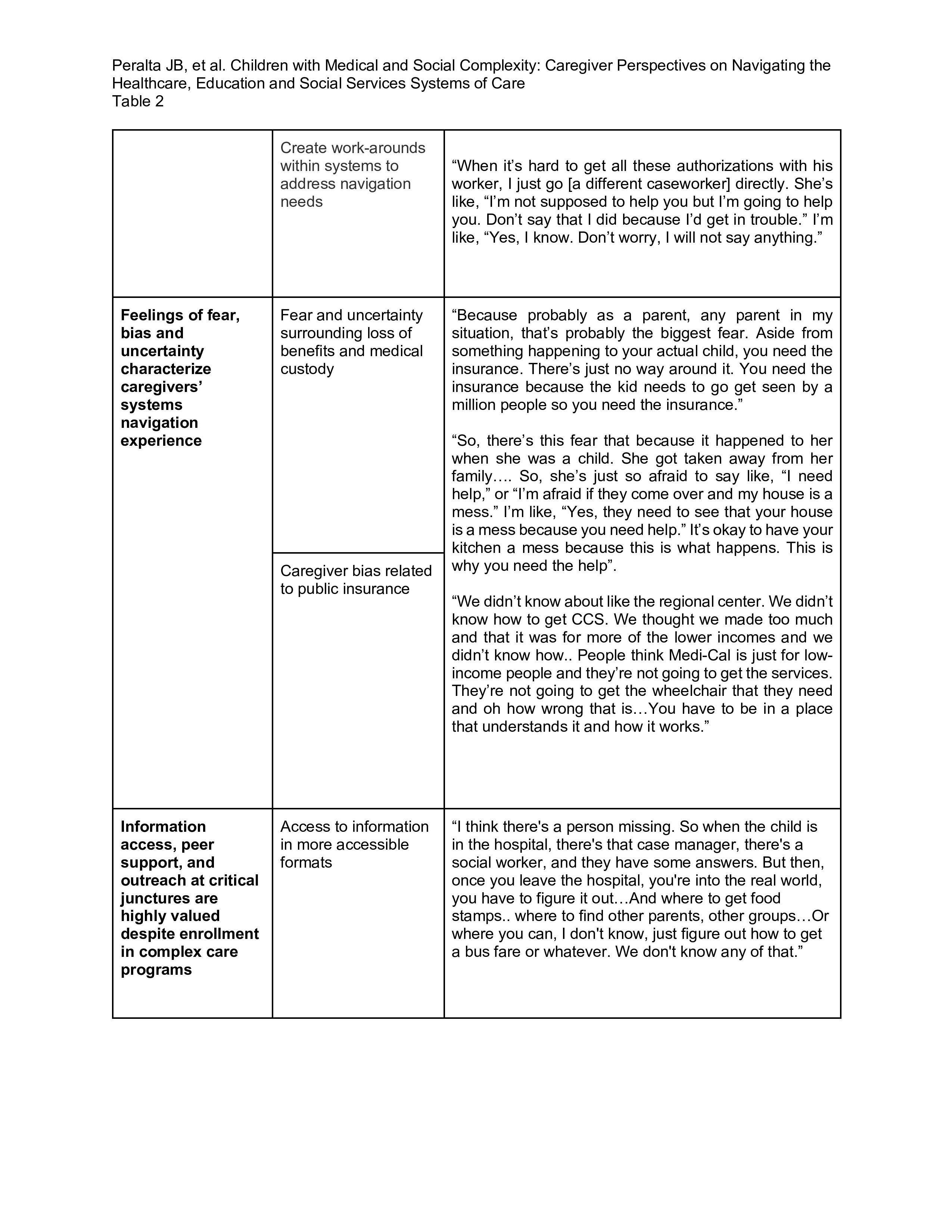
Results: Four key themes emerged: 1) Systems inefficiencies and failures exacerbate unmet social needs and increase the care burden particularly among families with severe medical complexity and caregiver health needs; 2) Public assistance programs and policies fail to meet the unique medical and socioeconomic needs of CMC+SC families; 3) Feelings of fear, bias and uncertainty characterize caregivers’ systems navigation experience; and 4) Information access, peer support, and outreach at critical junctures are highly valued beyond enrollment in complex care programs. Unmet social needs related to finances and their child’s education and insurance coverage were most common.
Conclusion(s): Family-serving systems of care may inadvertently exacerbate social complexity and caregiving responsibilities experienced by CMC+SC families. Current complex care and public assistance programs are insufficient to address complex needs experienced by CMC families with social complexity. Targeted interventions that increase information access and opportunities for caregiver peer support may improve wellbeing for these CMC+SC caregivers and their children.
.jpg)