Global Neonatal & Children's Health
Session: Global Neonatal & Children's Health 1
473 - Assessing Physician-Perceived Barriers Contributing to Delayed Presentation of Childhood Cancer in Vietnam: A Nationwide Survey
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 473
Publication Number: 473.339
Publication Number: 473.339

Paul Phan (he/him/his)
Medical Student
Johns Hopkins University School of Medicine
Nottingham, Maryland, United States
Presenting Author(s)
Background: Limited awareness and access to care cause many children in low-to-middle-income countries (LMICs) to be misdiagnosed or receive delayed treatment. Primary care providers (PCPs) and cancer specialists are instrumental in detecting early cancer symptoms and referring patients to advanced treatment, but little research has focused on the challenges that these physicians encounter when diagnosing children with cancer in LMICs.
Objective: This study aims to understand the physician-perceived barriers that impact the quality and timeliness of pediatric cancer screening and treatment in Vietnam.
Design/Methods: A 35-question structured questionnaire in Vietnamese was distributed online as an anonymous Qualtrics survey. PCPs and cancer specialists with experience caring for children were targeted through nationwide mailing lists and social media. Questions collected information on demographics and previous training. A five-item Likert Scale assessed agreeability to questions regarding child cancer knowledge, organizational factors, and educational needs. Data was analyzed using descriptive statistics.
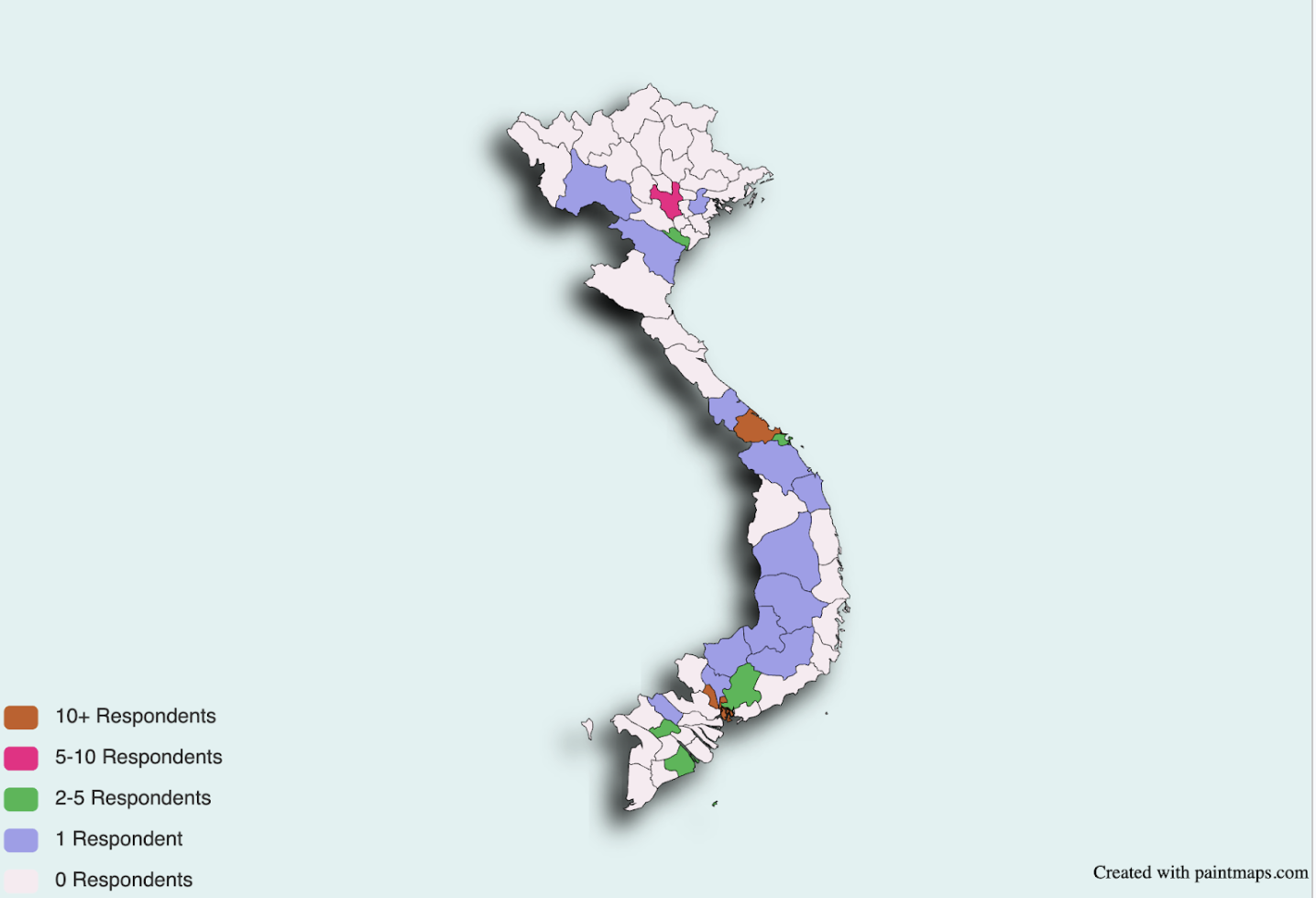
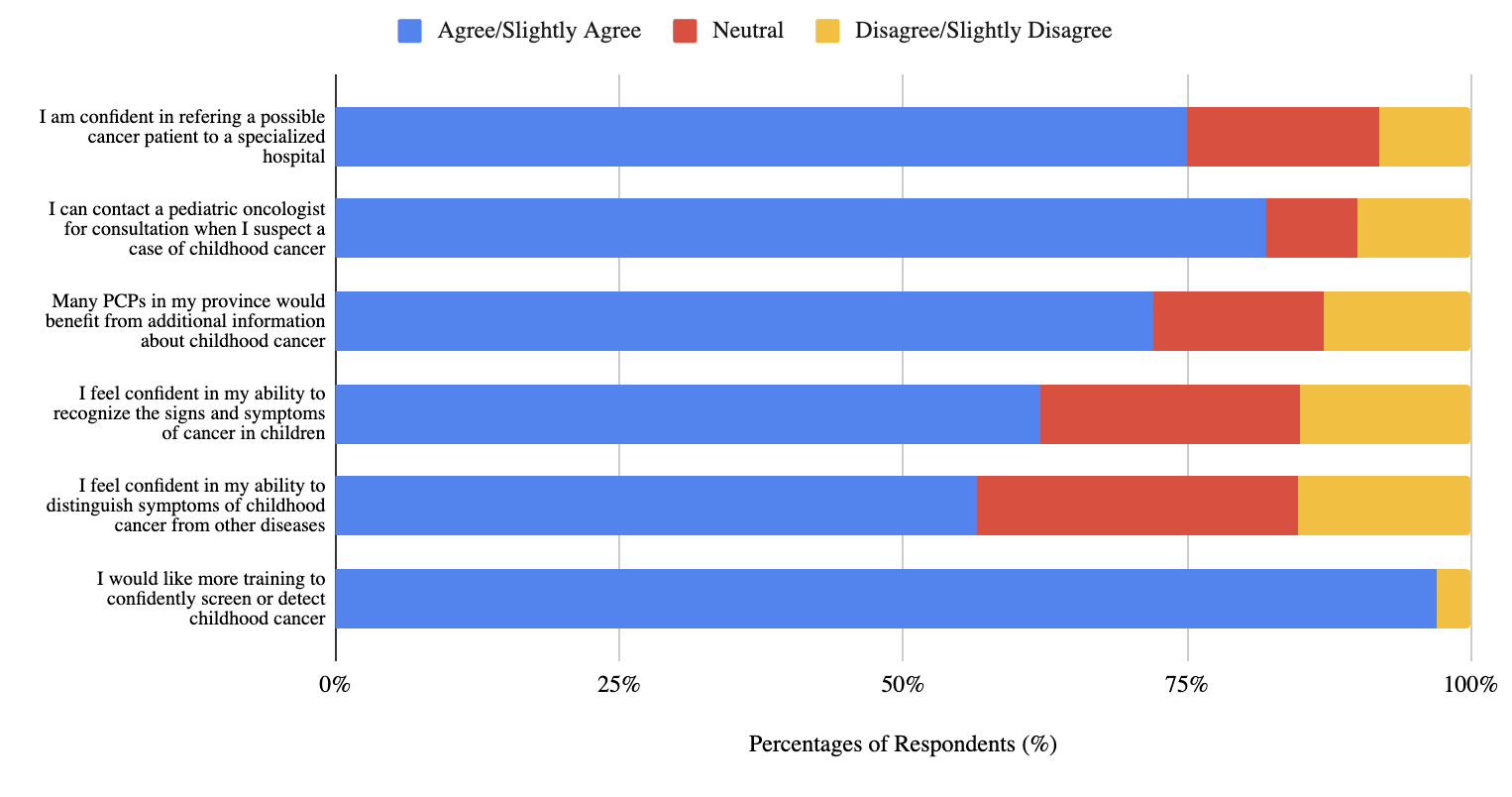
Results: 105 physicians, representing 22/58 (38%) Vietnamese provinces, responded to the survey. 51 (49%) respondents self-identified as PCPs, 23 (22%) as hematologists/oncologists, and 4 (4%) as surgeons. Among PCPs, 31% had not previously screened a child for cancer. Only 62% reported being able to recognize early cancer signs and symptoms, and 56% felt confident in distinguishing cancer from other conditions. Across all specialties, less than 11% of physicians correctly answered a knowledge question regarding the curability of pediatric Acute Lymphoblastic Leukemia, and 94% expressed a need for more education on cancer detection. Furthermore, a slight majority of all physicians reported that their facilities had adequate infrastructure (58%) and supplies (57%) to screen or diagnose children for cancer. At the patient level, physicians report that following screening/diagnosis, travel distance (85%), limited financial resources (89%), and low familial support (74%) are key factors impeding their patients from receiving cancer treatment.
Conclusion(s): Vietnamese doctors underestimate childhood leukemia as a curable disease and desire increased training on cancer detection. Expanding child cancer-specific education among physicians and addressing patient- and facility-level factors may facilitate more timely and adequate diagnosis and treatment. Qualitative interviews are being conducted to better understand how physicians in Vietnam and other LMICs can be supported to best care for children living with cancer.
.png)
