Emergency Medicine
Session: Emergency Medicine 11: Potpourri
409 - Feasibility, Acceptability, and Potential Effectiveness of Audio Discharge Instructions for Optimizing Outcomes after ED Discharge: The RECORD-ED Pilot Study
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 409
Publication Number: 409.3142
Publication Number: 409.3142
- KL
K. Casey Lion, MD, MPH (she/her/hers)
Associate Professor
University of Washington/ Seattle Children’s Hospital
Seattle, Washington, United States
Presenting Author(s)
Background: Over 32 million US children live in a household with low income, low health literacy, or language barriers; they experience worse health outcomes. Language-concordant audio discharge instructions addresses language and literacy barriers and may promote review and better retention, facilitating improved outcomes.
Objective: We tested the feasibility, acceptability, and effectiveness of audio-recorded discharge instructions for children treated in the ED for wheezing using a physical recordable card or through the online patient portal.
Design/Methods: We enrolled parents of children age < 10 with Medicaid insurance, whose language was English or Spanish, and were discharged following ED treatment for wheezing. Parents were randomized to usual care or usual care plus standard, pre-recorded audio-instructions accessed via a physical card (PC) or through a patient portal link (PP). Audio instructions were developed in multi-disciplinary design workshops including parents, in each language. Parents completed surveys at ED enrollment and follow-up: 2-3 days, 7-10 days, and 3 months. Discharge instructions were abstracted from the medical record; concordance between provider- and parent-report was rated by 2 blinded coders. Differences by study arm were tested with chi-squared and t-test.
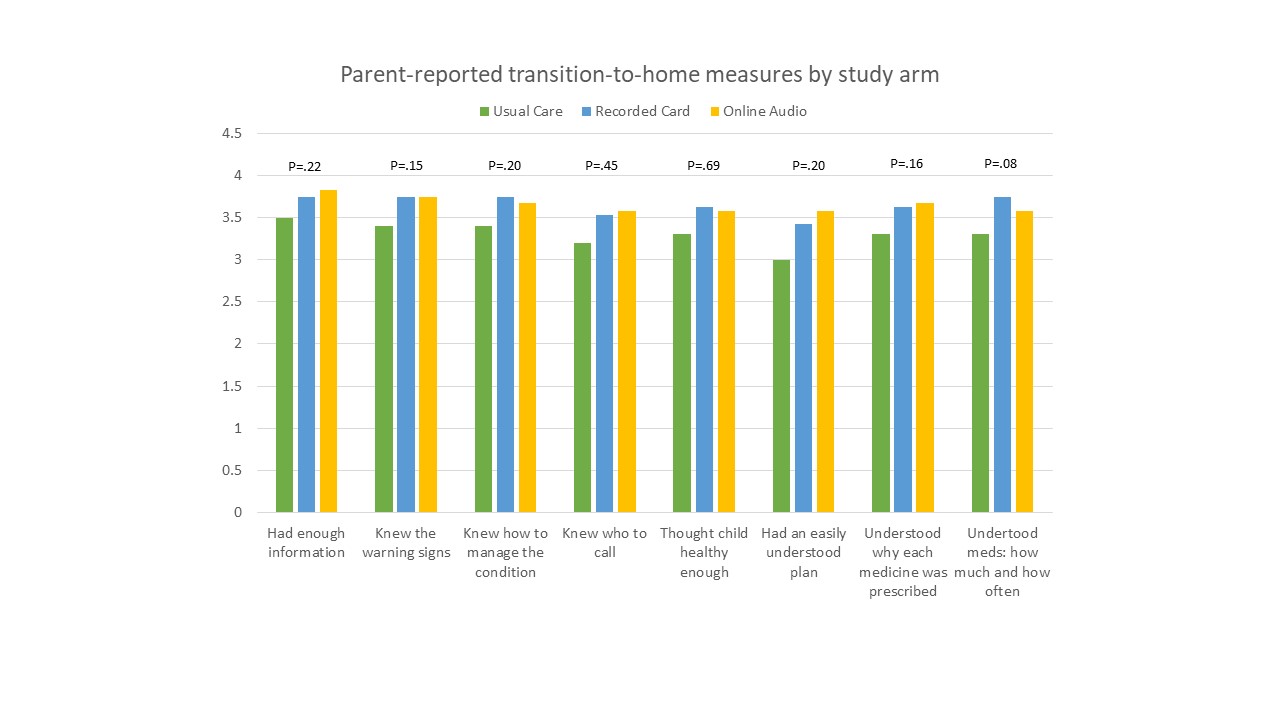
Results: Of 177 families approached from 12/2020 to 4/2022, 80 families enrolled and were randomized (45%). Sixteen percent (13/80) of families used Spanish for care, 83% of parents had less than a college degree, and 65% reported an annual income <$40,000. Follow-up survey completion rates were 51%, 50% and 44% for the 1st, 2nd, and 3rd surveys, respectively, without variation by arm. PC assigned parents reported more frequent use of audio instructions compared to PP: 71% (12/17) of parents with PC reported listening to instructions ≥1 time, 35% listened 2-5 times; 41% shared them with another person. In contrast, 55% (5/11) of parents with PP instructions reported listening, and none >1 time; 18% shared them with others. Parent-reported transition-to-home measures did not differ significantly by study arm (Figure). Parents correctly named 34% of discharge instructions across 3 domains (medications, follow-up, return precautions), with no difference by arm.
Conclusion(s): We found audio-recorded instructions to be acceptable to parents, with physical cards demonstrating more use than patient portal access. Instruction recall was low. We were unable to demonstrate feasibility and potential effectiveness during this pilot due to pandemic-related recruitment and retention challenges.