Nephrology
Session: Nephrology 4
20 - Diet Restrictions in Kidney Disease: Exploring the Role of Food Insecurity on Adherence and Outcomes
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 20
Publication Number: 20.1802
Publication Number: 20.1802

Zecilly Guzman, BA (she/her/hers)
Behavioral Research Coordinator
Ann & Robert H. Lurie Children's Hospital of Chicago
Chicago, Illinois, United States
Presenting Author(s)
Background: Food insecurity (FI) is prevalent among children with chronic kidney disease (CKD) and may be an important mediator in the socioeconomic disparities seen in CKD outcomes. Little is known about the role FI plays in children with CKD and its impact on prescribed diet restrictions.
Objective: A mixed-methods single center cohort study exploring the relationship between FI, adherence to diet restrictions, and outcomes for children with CKD.
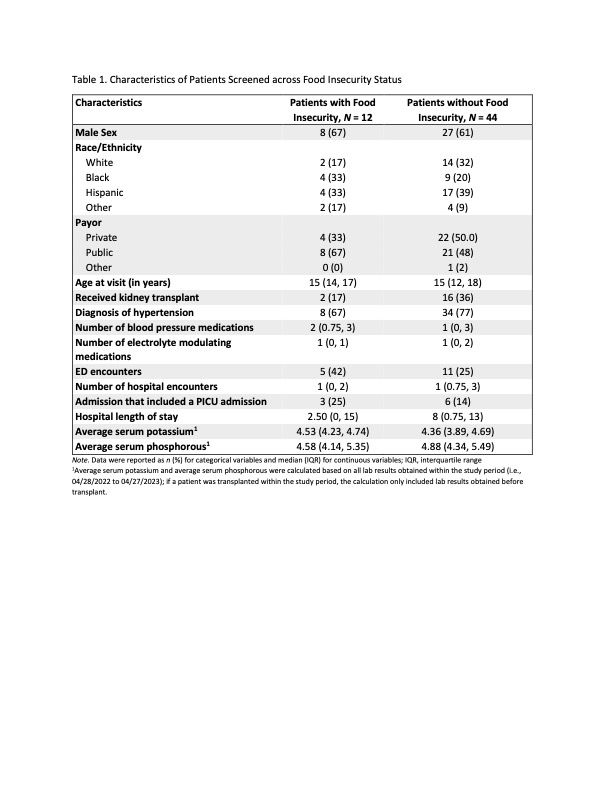
Design/Methods: All patients seen with a diagnosis of advanced CKD or end stage kidney disease (stage 4, 5, or 5d) from April 2022 to April 2023 were eligible for participation. Demographic, socioeconomic status, and CKD specific outcomes of interest were compared across FI status; then associations between FI and CKD outcomes were explored using multivariable linear or logistic regression. We conducted a qualitative sub-analysis where de-identified parent/guardian interview transcripts were analyzed for themes around prescribed diet restrictions with a special focus on the role of FI.
Results: FI compared to non-FI patients were more likely to be of Black race (33% vs 20%); have public insurance (67% vs 48%); need more blood pressure medications (2 [0.75,3] vs 1 [0,3]); and have a higher likelihood of an emergency department (42% vs 25%) or intensive care unit encounter (25% vs 14%). There were no associations of FI and outcomes of interest identified in multivariate regression. Four major themes emerged from parent/guardian interviews: 1. Family’s understanding of the renal diet focuses on foods to avoid; 2. Adapting to suggested dietary restrictions requires a change in grocery shopping and meal preparation at home; 3. Challenges around adherence include social stigma, emotional response of the child, and concerns around growth, budget, and time, and 4. Resources to help adherence involve improved food labels and increased public awareness of kidney disease.
Conclusion(s): Children with FI are at risk for higher medical needs. Adhering to prescribed diet restrictions in kidney disease involves significant dedication of time, resources, and funds. Challenges involve availability and affordability of appropriate foods, a child’s response to set restrictions, and social stigma. These results should guide future larger multicenter studies and interventions addressing food insecurity in the kidney disease population.