Hypertension
Session: Hypertension
59 - A Four-Year Study of Hypertension Diagnosis in Children: Comparison of In-Office Blood Pressure and Ambulatory Blood Pressure Monitoring in 200 Patients at a Single Institution
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 59
Publication Number: 59.1699
Publication Number: 59.1699

Faruk Oktem, MD (he/him/his)
Pediatric Nephrology Fellow
Jacobs School of Medicine and Biomedical Sciences at the University at Buffalo
Amherst, New York, United States
Presenting Author(s)
Background: Pediatric hypertension (HTN) affects 5 % of the child population, with potentially severe neurocognitive and cardiovascular consequences in adulthood. Effective blood pressure (BP) control is paramount. Ambulatory blood pressure monitoring (ABPM) has gained recognition over the past two decades. In 2014, the American Heart Association published guidelines for hypertension diagnosis in pediatrics, which were updated in 2022, necessitating a comprehensive evaluation.
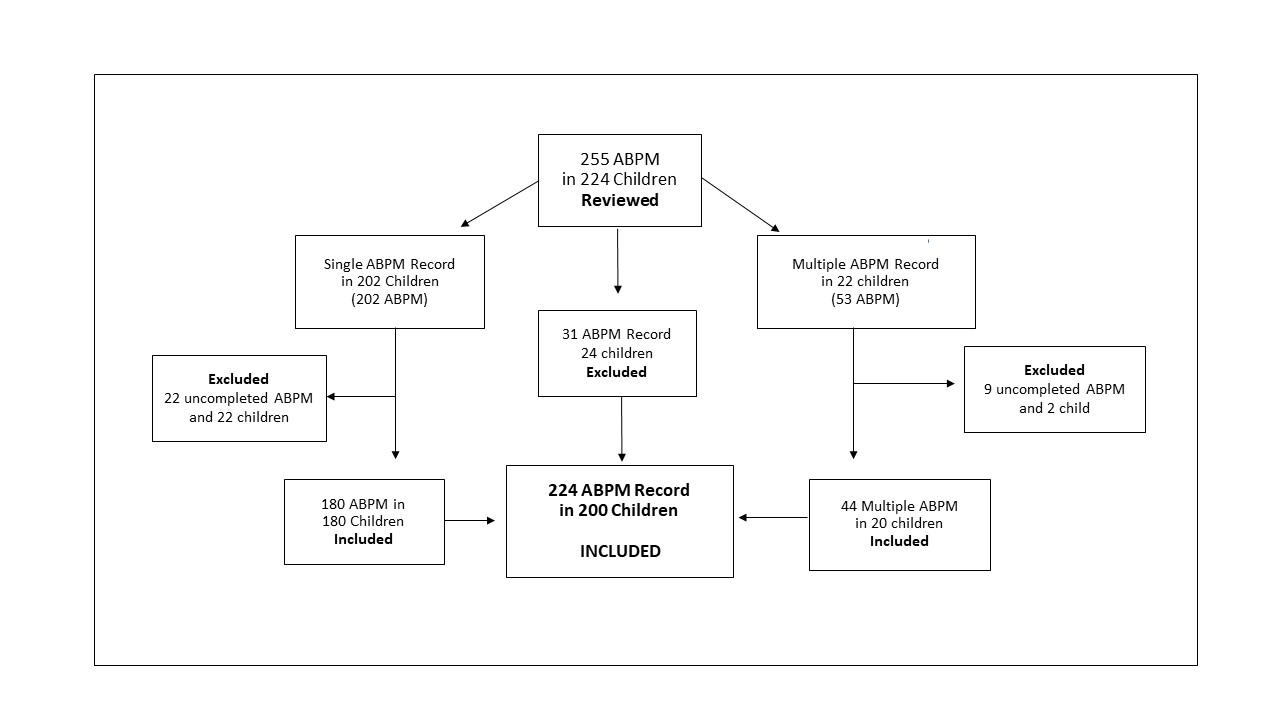
Objective: This four-year retrospective study, conducted at a single institution, involved 200 pediatric patients, totaling 224 ABPM studies. Our study aimed to compare in-office blood pressure (OBP) with ABPM for pediatric HTN diagnosis and to assess the impact of the 2022 guidelines on ABPM diagnoses compared to the 2014 guidelines.
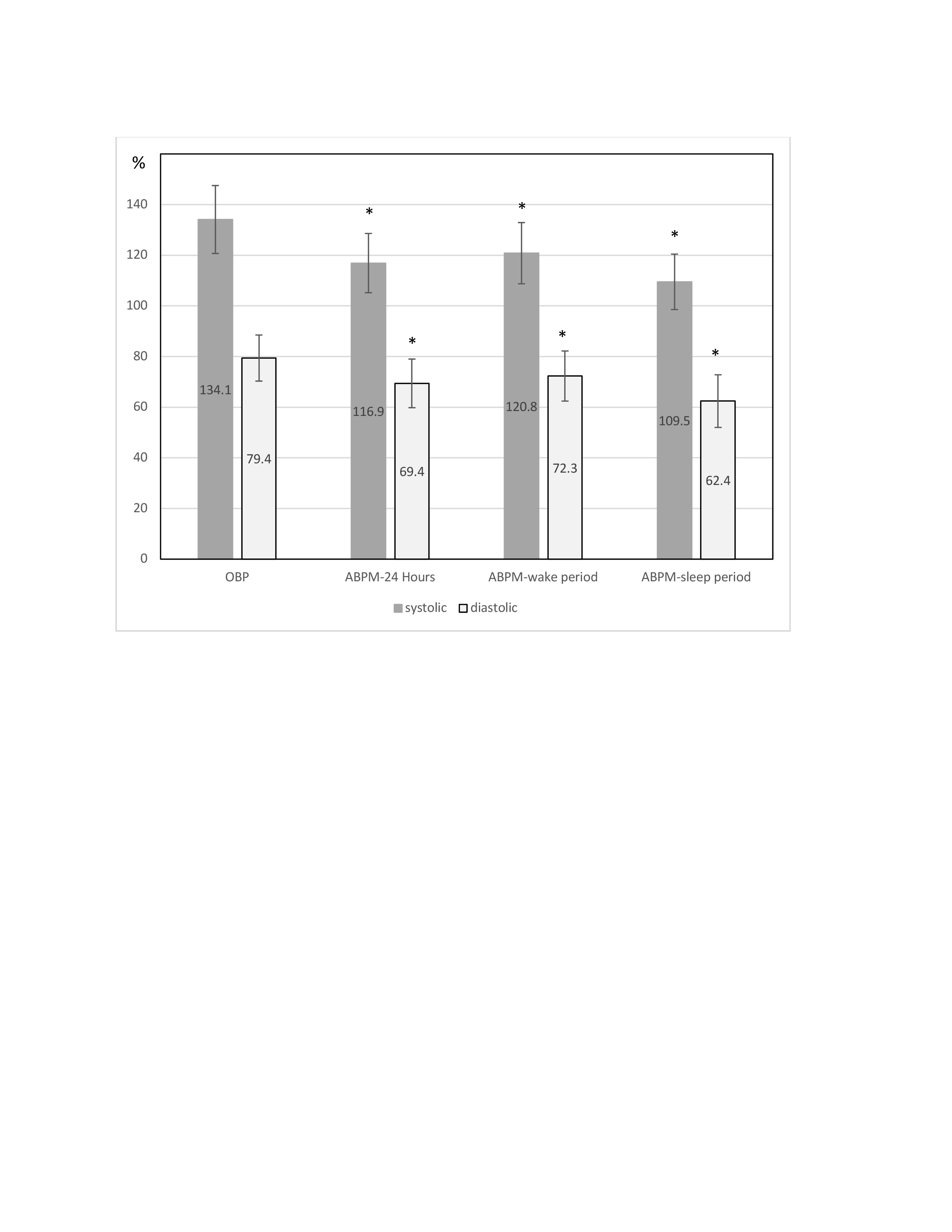
Design/Methods: Patients were analyzed in terms of relevant characteristics such as gender, BMI, eGFR, CKD, diabetes, dialysis, and kidney transplant status. We compared OBP readings with ABPM measurements taken over 24 hours, during wake and sleep periods. OBP readings were obtained using automated oscillometric devices, while ABPM records were collected at 20-minute intervals during the day and 30-minute intervals at night.
Results: Among 200 patients studied, 58 % were obese (BMI≥25), 6 % had CKD stages III-V (GFR < 60), 7 % exhibited left ventricular hypertrophy, and 6 % were kidney transplant recipients. Out of 255 ABPM records, 31 (12%) were unsuccessful. The remaining 224 records, spanning ages 5 to 20 years, comprised 62 % males, 37 % females, and 1 % transgender individuals (Figure 1). Notably, OBP measurements (systolic and diastolic BP) were significantly higher compared to ABPM (24 hours, wake period, and sleep period), highlighting the prevalence of white coat HTN detectable through ABPM (Figure 2, p< 0.001). Under the 2014 guidelines, 110 patients were diagnosed with white coat HTN, 5 with masked HTN, and 46 with sustained HTN. In contrast, the 2022 guidelines identified 93 cases of white coat HTN, 16 of masked HTN, and 91 of sustained HTN. These findings underscore the enhanced sensitivity of the 2022 guidelines in detecting masked and sustained HTN (Figure 3, p< 0.001).
Conclusion(s): ABPM emerges as a valuable tool for identifying "white coat" HTN compared to OBP. The 2022 ABPM guidelines significantly improve HTN diagnosis, particularly in the detection of masked and sustained HTN, reaffirming ABPM's role as the gold standard for HTN diagnosis. Further research is warranted to assess the clinical implications of these new guidelines on ABPM outcomes.
.jpg)
