General Pediatrics
Session: General Pediatrics 3
349 - Piperacillin/Tazobactam versus Ceftriaxone and Metronidazole for Children with Perforated Appendicitis: A Systematic Review and Meta-analysis
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 349
Publication Number: 349.1672
Publication Number: 349.1672

Jennifer Armstrong, MSc (she/her/hers)
Student
Meharry Medical College
Burlington, Ontario, Canada
Presenting Author(s)
Background: The management of perforated appendicitis includes laparoscopic appendectomy followed by postoperative intravenous antibiotics. In the United States and Canada, the most common regimens for children are Piperacillin/Tazobactam (PT) or Ceftriaxone and Metronidazole (CM).
Objective: We conducted a systematic review and meta-analysis of postoperative PT versus CM for children with perforated appendicitis.
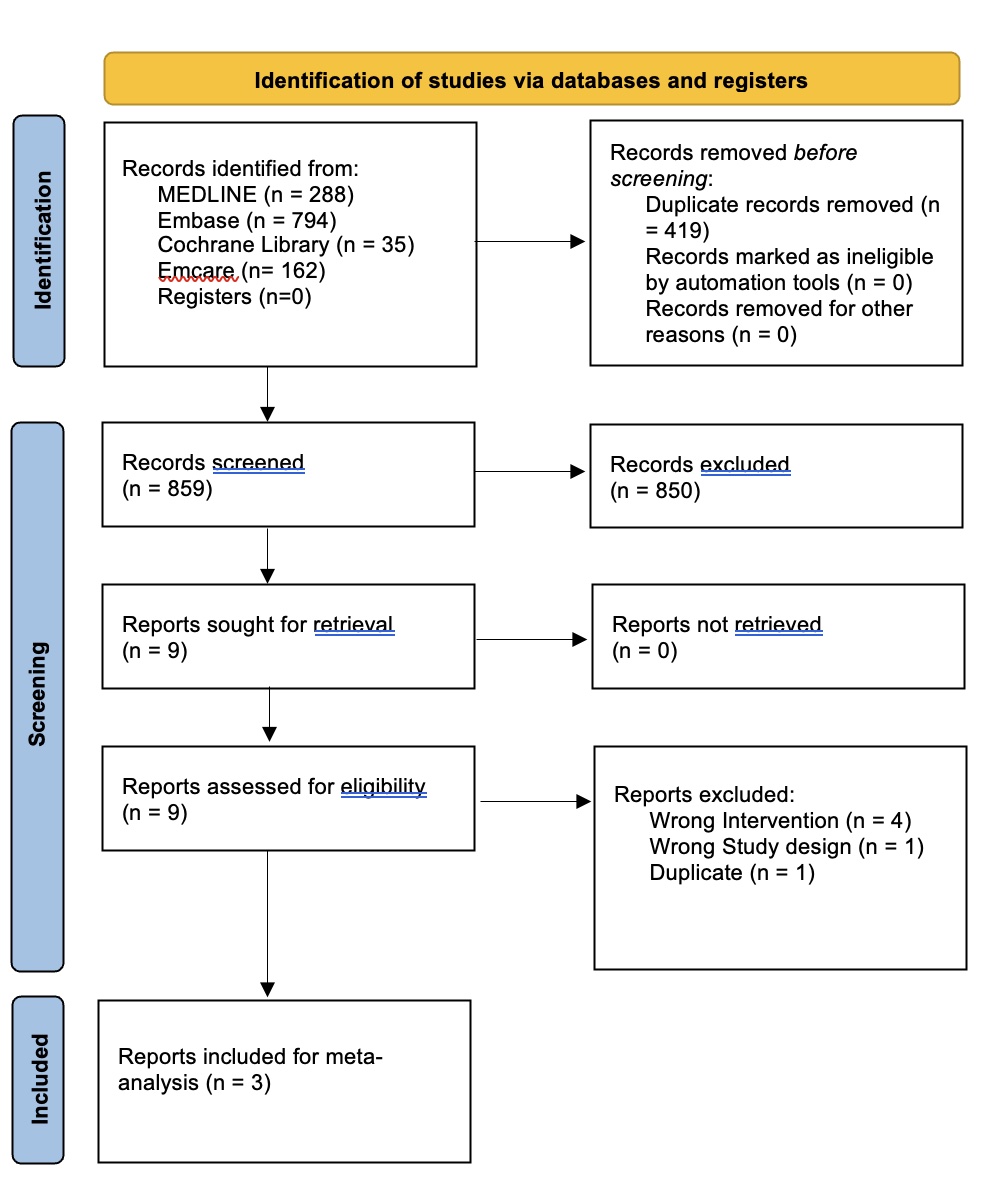
Design/Methods: The protocol for this review was registered with the International Prospective Register of Systematic Reviews. A medical librarian completed structured searches of Medline, Embase, Emcare, and Cochrane from 1990 to June 2023. Two authors screened abstracts, reviewed full-text manuscripts, and extracted data in duplicate. Outcome data were meta-analyzed in RevMan using a random effects model. Studies were stratified by study design and summary statistics were reported using relative risk (RR) and 95% confidence intervals. Risk of bias was assessed using the Cochrane Tool (RoB 2) for randomized controlled trials (RCT) and the Newcastle-Ottawa Scale for observational studies.
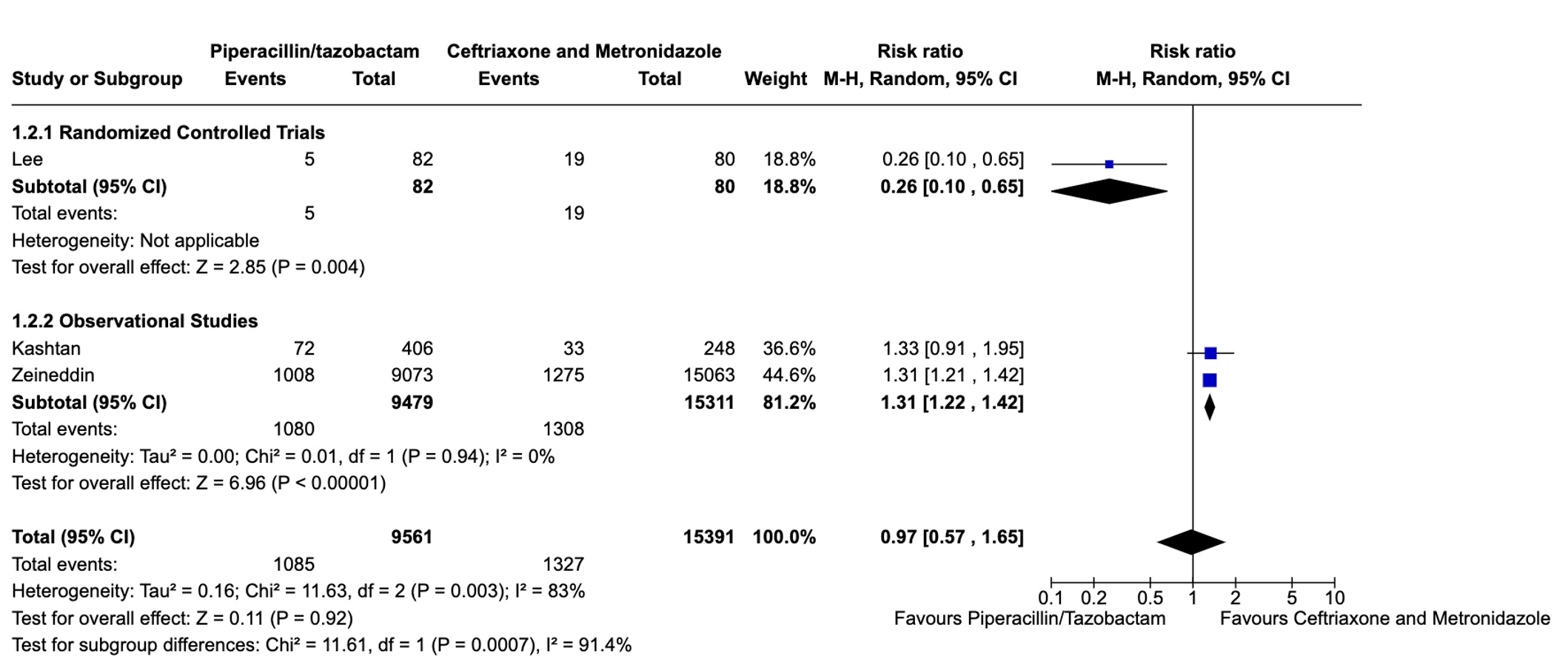
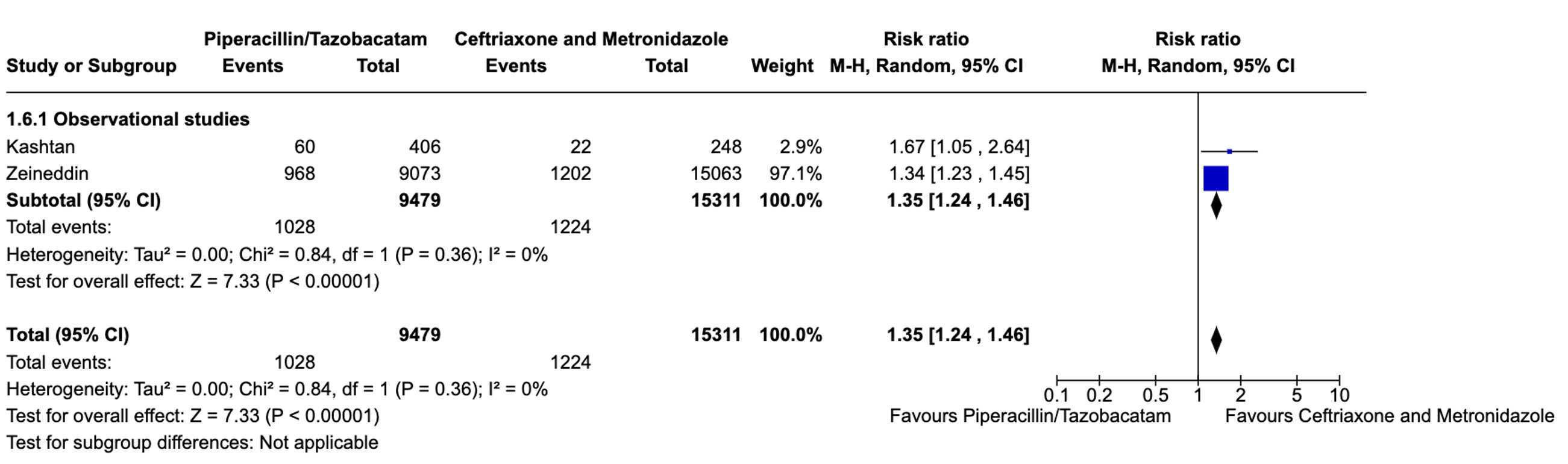
Results: We identified one non-blinded RCT with 162 children with perforated appendicitis and two comparative, multicenter, observational studies with 29,667 children. All participants underwent laparoscopic appendectomy and received postoperative PT (n=9,561) or CM (n=15,391). Meta-analyses revealed considerable heterogeneity between the results of the RCT and the two observational studies. In the RCT, children treated with PT had decreased risk of deep surgical site infection, postoperative imaging, and return to the emergency department. In the observational studies, however, the treatment effect was reversed and improved outcomes were seen with CM. The overall treatment effect suggested no difference between PT and CM in terms of deep surgical site infection (RR=0.97, 0.57-1.65), postoperative imaging (RR=0.99, 0.71-1.37), return to the emergency department (RR=0.82, 0.50-1.37), and readmission to hospital (RR=0.85, 0.45-1.62). The heterogeneity for these outcomes was substantial with I2 statistics ranging from 73-83%. The RCT was limited by lack of blinding and not reporting percutaneous drain insertion. One observational study was limited by the use of administrative data only.
Conclusion(s): The best antibiotic regimen for children with perforated appendicitis remains uncertain. One non-blinded RCT showed improved outcomes with PT, but two large, observational studies favored CM. There is a need for a trial with adequate blinding and outcome reporting, especially percutaneous drain insertion.