Medical Education
Session: Medical Education 5
414 - Research Training and Scholarly Activity during Pediatric Residency: A Cross Sectional Survey of Canadian Pediatric Residents
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 414
Publication Number: 414.1670
Publication Number: 414.1670
- JL
Jimin Lee, MD, MS
Assistant Professor
Weill Cornell Medicine
New York, New York, United States
Presenting Author(s)
Background: Pediatric residents must receive research training and conduct scholarly projects during residency. However, substantial variability exists in how these competencies are achieved between residency programs in Canada without standardized expectations.
Objective: This study aimed to describe the characteristics of research training and scholarly activity (SA) during pediatric residency and identify facilitators and barriers to resident SA.
Design/Methods: We conducted a cross-sectional survey of pediatric residents from all 17 pediatric residency programs across Canada from April to June 2023. We collaborated with medical education experts to develop a 55-item survey with multiple-choice and open-ended questions, pilot tested, and distributed electronically to residents through program directors (PDs). The questions included demographics, career interests, SA type and progress, satisfaction with research training, and barriers and facilitators to resident SA. Responses were complemented with program-level data from the PDs. Data were analyzed using descriptive statistics. Residents’ self-reported progress on SA was compared with the expected “on-track” progress for their postgraduate year based on PD responses. We used conventional content analysis to code the qualitative data from open-ended responses.
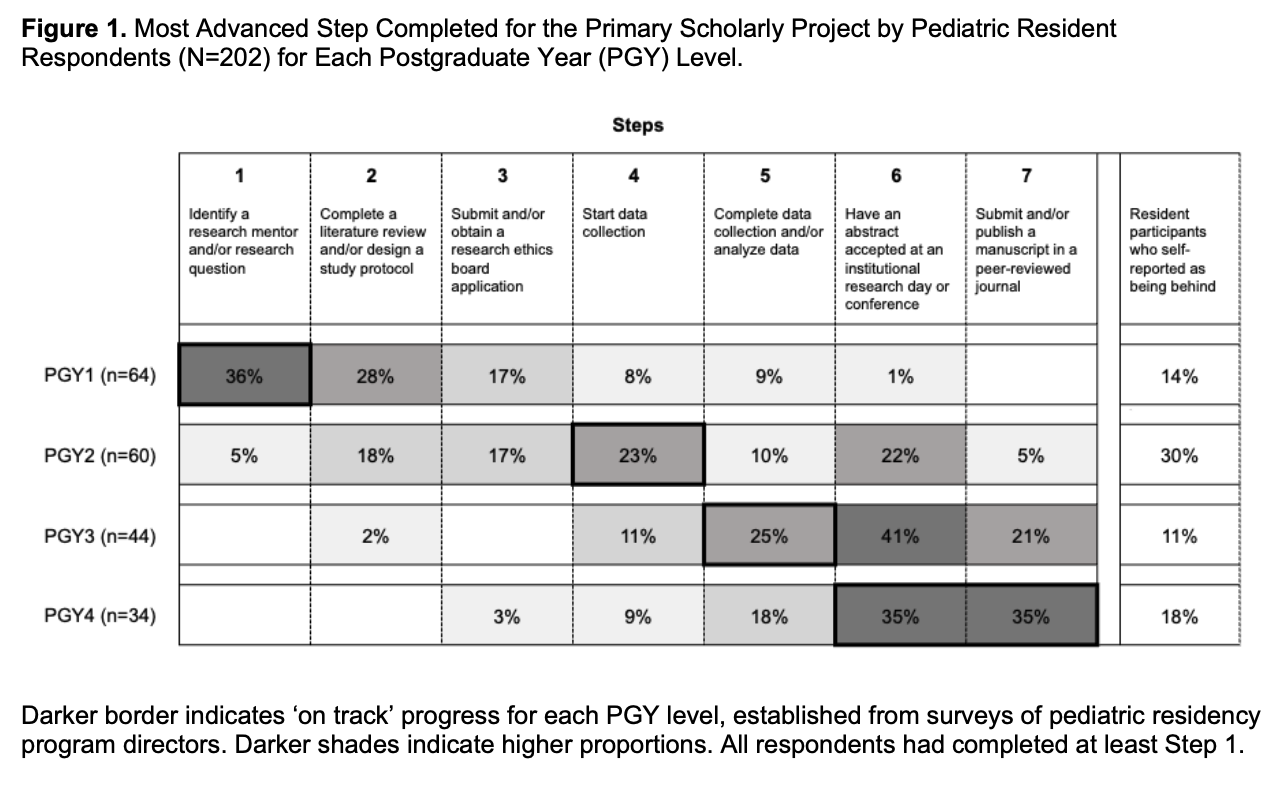
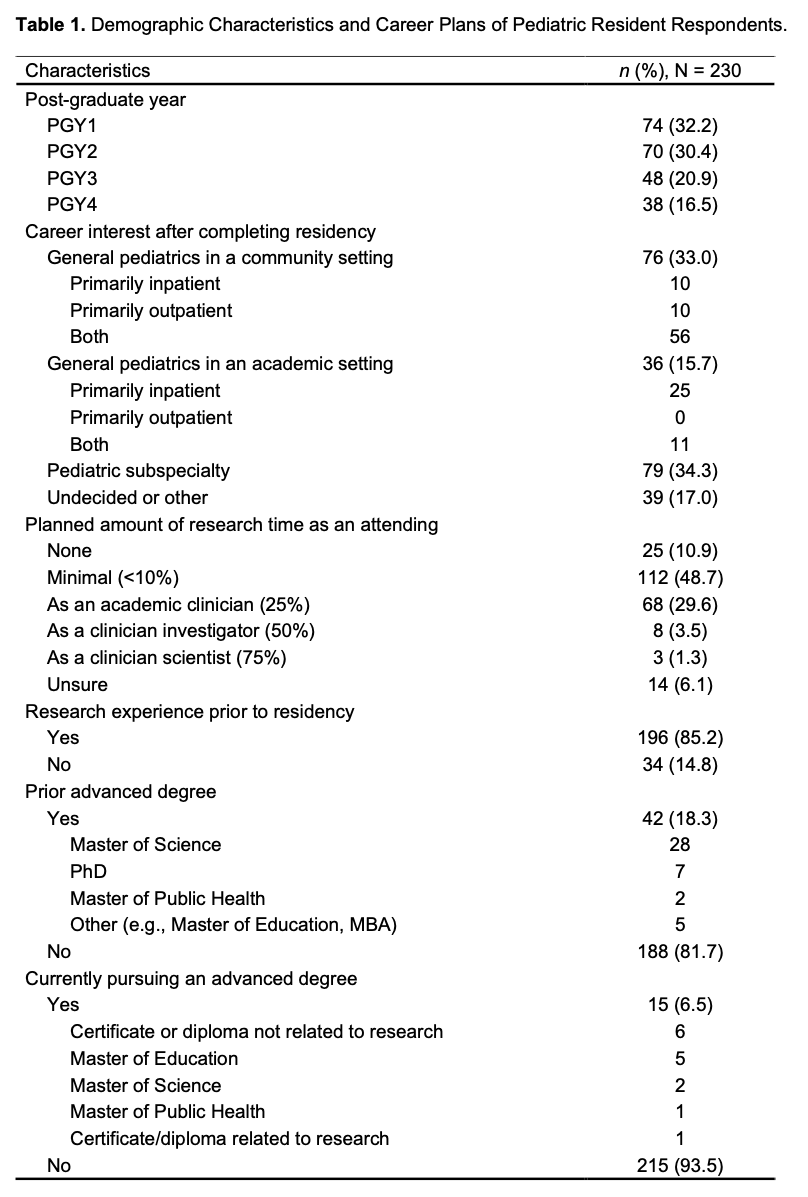
Results: Of 644 Canadian pediatric residents, 230 (36%) responded. All 17 PDs completed the survey. Only 5% of resident respondents intended to spend ≥50% of their time on research as attending physicians, and most of them were interested in pediatric subspecialty training (Table 1). Residents conducted various types of SA, including retrospective clinical study (22%), qualitative research (15%), and quality improvement (13%). Among respondents, 20% had abstracts accepted at national or international conferences, and 12% had manuscripts submitted to peer-reviewed journals. Overall, 61% of respondents reported being satisfied with research training during residency. At each PGY level, there was a wide range of completed steps for SA (Fig 1). Residents’ self-perceived compared to actual progress (ahead, on track, or behind) in their SA were discrepant in 15% of cases. Key themes related to barriers and facilitators to SA included protected time for research, mentorship, and research skills training (Table 2).
Conclusion(s): The scholarly activity experience of pediatric residents in Canada is highly variable. Establishing national standards, implementing progress monitoring mechanisms with tailored support, and offering flexible protected research time are important next steps.
.png)