Neonatology
Session: Neonatal Follow-up 3
536 - Impact of Pre-NICU Discharge Contact with NICU Follow-up Provider on Compliance with Feeding Recommendations at Initial Clinic Visit
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 536
Publication Number: 536.2729
Publication Number: 536.2729

Emily Scott, MD, MS (she/her/hers)
Associate Professor of Clinical Pediatrics
Indiana University School of Medicine
Indiana University School of Medicine
Indianapolis, Indiana, United States
Presenting Author(s)
Background: While families eagerly anticipate their child’s discharge from the neonatal intensive care unit (NICU), the transition from NICU to home can nonetheless be challenging. NICU graduates often require additional feeding support, such as enteral tubes and fortified feeds, in the home environment. Our NICU follow-up program manages feeding for NICU graduates. Clinic providers often find that families have discontinued enteral tube feeds or changed formula mixing prior to their first follow-up visit 2-4 weeks after discharge. This can have a significant impact on an infant’s health, growth and development
Objective: This is a prospective cohort study to determine whether a structured discussion prior to NICU discharge between the family and an advanced practice provider (APP) from the NICU follow-up team improves attendance at first NICU follow-up visit and compliance with discharge feeding plan.
Design/Methods: The APP is notified through secure messaging about an upcoming discharge. The APP contacts the family to set up an in person meeting in the NICU prior to discharge. If family is unable to meet with the APP at bedside, a phone meeting is be scheduled. A structured discussion is led by the APP reviewing topics such as formula mixing, nipple flow rate – in addition to introducing the NICU follow-up program, reinforcing safe sleep and educating families on when to seek urgent medical care. (Figure 1) Data around notification, completion of contact and status at follow-up are collected on a secure Excel spreadsheet and SPSS Statistics is used to perform chi-square tests.
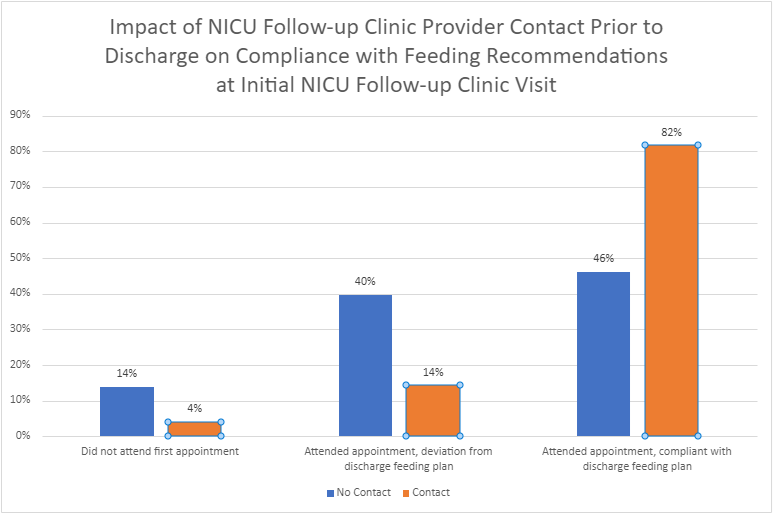
Results: Since implementation in March 2023 to current date, 147 patients were discharged to our NICU follow-up program. APP completed structured discussion with 53 (36%) of these patients prior to NICU discharge. 42% of these discussions were held in person; 58% were completed via telephone. Compared to the 94 patients who did not have pre-discharge contact, families who met with the NICU follow-up APP were significantly more likely to attend their first follow-up appointment (96% vs. 86%) and be compliant with their discharge feeding plan (82% vs. 46%) (p < 0.01). (Figure 2)
Conclusion(s): Pre-discharge contact with an APP from the NICU follow-up team increases attendance at the first follow-up appointment and compliance with the discharge NICU feeding plan, smoothing the transition home for patients and families. Next steps include utilizing QI methodology to increase the number of families who meet with the APP prior to discharge and assessing family satisfaction with the pre-discharge contact process.
.png)