Neonatology
Session: Neonatal Quality Improvement 4
58 - Cost savings of a sustained zero CLABSI rate using a dedicated NICU PICC team
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 58
Publication Number: 58.2725
Publication Number: 58.2725

Susan M. Bedwell, susan-bedwell@ouhsc.edu (she/her/hers)
Director of Quality, Neonatal-Perinatal Services
Oklahoma Childrens Hospital at OU Health
Guthrie, Oklahoma, United States
Presenting Author(s)
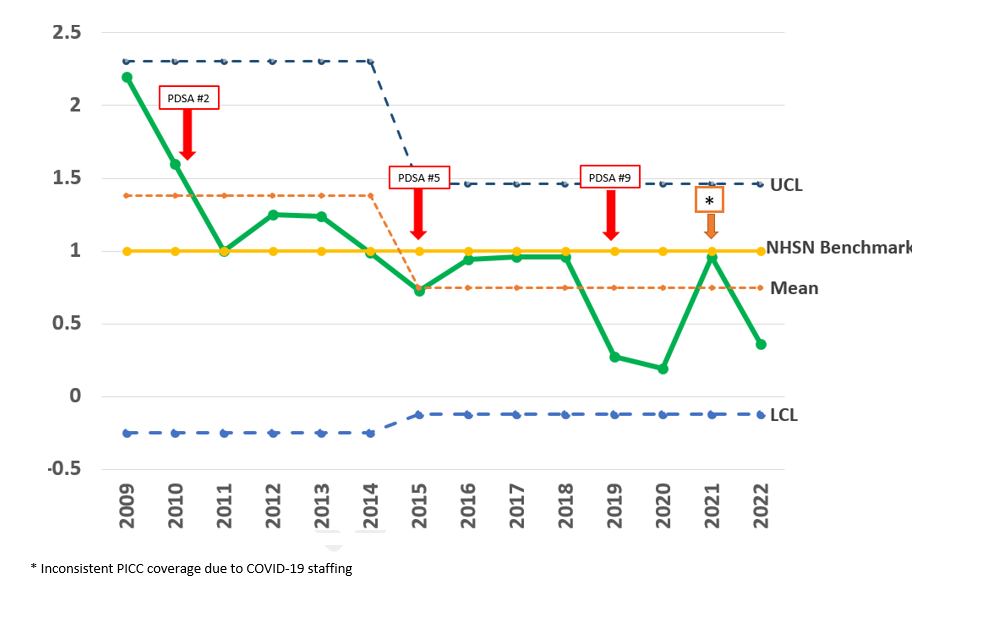
Background: Neonatal central line-associated bacteremias (CLABSIs) cost approximately $90,122 per event and increase the length of stay by approximately 19 days. Premature infants who experience a CLABSI have higher mortality rates, poor growth, and more neurodevelopmental complications. In our neonatal intensive care unit prior to 2009, nurses trained in peripherally inserted central line catheter (PICC) placement were often pulled out of patient care to insert lines. All bedside nurses were expected to perform PICC line maintenance including dressing and cap changes. The CLABSI rate in 2009 was more than twice the NSHN average at 2.42 per 1000-line days representing 23 events in 9500-line days.
Objective: The aim of the project was to reduce and sustain the NICU CLABSI rate below the CDC NHSN benchmark of 1.
Design/Methods: With physician and nursing leadership support, the clinical nurse specialist (CNS) guided the unit from on-demand PICC placement to dedicated PICC hours, where a team of 7-10 PICC-certified nurses split their work time between patient care and dedicated PICC days. PICC team responsibilities include placement and adjustment of PICC lines, central line dressing changes, cap lock replacement, and central line blood draws. With the guidance of the CNS, the team drives quality projects for the prevention of CLABSIs, develops policies, educates staff, and teaches medical fellows proper PICC line techniques, The teams’ informal leadership among the NICU staff allows for rapid-cycle quality improvement and the adoption of evidence-based practices with an immediate impact on patient outcomes.
Results: The initiative took 6 PDSA cycles to reach a CLABSI rate of zero. CLABSI reduction interventions saved approximately 2.9 million dollars in related CLABSI costs from 2015-2019 compared to 2010-2014. The team saved an additional $2.5 million in CLABSI-related costs from 2020 to 2023. The trend has been maintained even with an increase in line days (14,400 for 2022), and rising admissions of critically ill and ELBW infants. A zero CLABSI rate has been sustained since 2015. The unit had no reported CLABSIs for 465 days before having a single CLABSI in October 2023.
Conclusion(s): A dedicated APRN-led NICU PICC team achieves rapid cycle improvements that can lead to a zero CLABSI rate and subsequent cost savings in a large, Level 4 NICU. Nursing and physician leadership support is vital to sustain a dedicated PICC nurse position.