Neonatology
Session: Neonatal Nephrology/AKI 2
54 - Is Medication Management in the First 28 Days of Life Associated with Acute Kidney Injury in Extremely Low Birthweight Neonates?
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 54
Publication Number: 54.2288
Publication Number: 54.2288

Shannon K. Haines, MD, FAAP (she/her/hers)
Fellow of Neonatal-Perinatal Medicine
University of Nebraska College of Medicine
Papillion, Nebraska, United States
Presenting Author(s)
Background: Acute kidney injury (AKI) in extremely low birthweight (ELBW) infants is associated with increased risk of morbidity and mortality. The reasons for observed worsened health outcomes after injury aren’t fully elucidated but could be due to co-morbid conditions such as sepsis, adrenal insufficiency, steroid use, diuretic use, or electrolyte derangements.
Objective: Thus, our group sought to evaluate associations between AKI during neonatal intensive care unit (NICU) hospitalization in ELBW infants and common pre- and postnatal medical treatments and laboratory values.
Design/Methods: An IRB-approved retrospective chart review of infants born < 1,000g admitted to a level III NICU was completed. Data on AKI, medical interventions, and laboratory values was collected. AKI was defined as a rise in serum creatinine of ≥ 0.3 mg/dL within 48 hours or creatinine level >1.6 mg/dL, >1.1 mg/dL, and >1.0 for infants corrected to < 28 weeks, 28-29, and 30-32 weeks gestation, respectively. After adjusting for Clinical Risk Index for Babies (CRIB II) scores, we evaluated the association of AKI and the following variables from day of life (DOL) 1-14 and 15-28: diuretic use, steroid use, antibiotic use, combined enteral + parenteral protein provision in g/kg/day, maximum creatinine level, maximum sodium level, and minimum sodium level. We also evaluated the association of AKI and vasopressor use in the first 10 DOL, maternal antibiotic use, maternal NSAID use, and diagnosis of maternal hypertension.
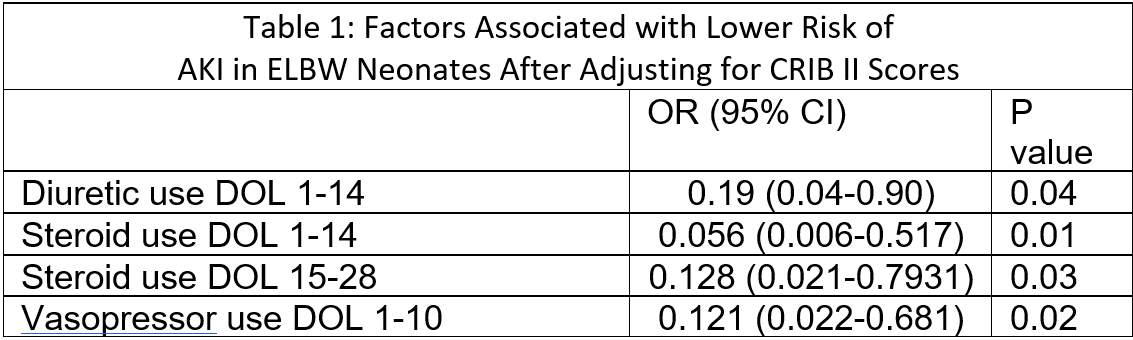
Results: After adjusting for CRIB II scores, infants who had vasopressor use on DOL 1-10; steroid use DOL 15-28; and diuretic use or steroid use on DOL 1-14 had lower odds of having an AKI after adjusting for CRIB II score (Table 1). No significant association was found between AKI and diuretic use DOL 15-28 or between AKI and antibiotic use, highest creatinine levels, highest or lowest sodium levels, or highest protein provision at DOL 1-14 and 15-28. The maternal factors of perinatal antibiotic use, recorded NSAID use, and hypertension were not associated with neonatal AKI.
Conclusion(s): The findings that diuretic, vasopressor, and steroid use were associated with lower odds of AKI were unexpected. We theorize this could be secondary to the prevention of volume overload or closer monitoring of the fluid status of these patients. A confounding factor could be that we did not define AKI by oliguria, which could affect the association between creatinine levels and steroid or diuretic use. Future research with a larger cohort is warranted to further study these associations and to identify medical interventions associated with AKI.