Hospital Medicine
Session: Hospital Medicine 5
158 - Social Risk Screening and Referrals in the Pediatric Inpatient Setting: The Current Landscape
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 158
Publication Number: 158.1106
Publication Number: 158.1106

Matthew S. Pantell, MD, MS (he/him/his)
Associate Professor
University of California, San Francisco, School of Medicine
San Francisco, California, United States
Presenting Author(s)
Background: Many professional organizations and regulatory bodies, including the American Academy of Pediatrics and the Children’s Hospital Association, endorse screening for social risk factors –social drivers/determinants of health (SDOH) associated with adverse health outcomes - in clinical settings. Additionally, the Joint Commission and National Committee for Quality Assurance are recommending screening for SDOH in hospital settings starting in 2024. Some studies have explored SDOH screening rates among children’s hospitals, but they lacked inclusion of other hospital types and details on screening domains and how hospitals respond to families with identified needs.
Objective: To describe social risk screening and referral practices among pediatric hospitals in a national sample.
Design/Methods: We collected data via a survey distributed through the Pediatric Research in Inpatient Settings Network (PRIS), a research network consisting of 92 hospitals (tertiary and community) in 43 states. PRIS contacts were emailed a copy of a survey asking about hospital SDOH practices between Aug-Nov 2023 and asked to have a knowledgeable contact complete it. Additionally, we emailed the survey to 4 community hospital affiliates identified by PRIS survey respondents. We calculated descriptive statistics of survey responses.
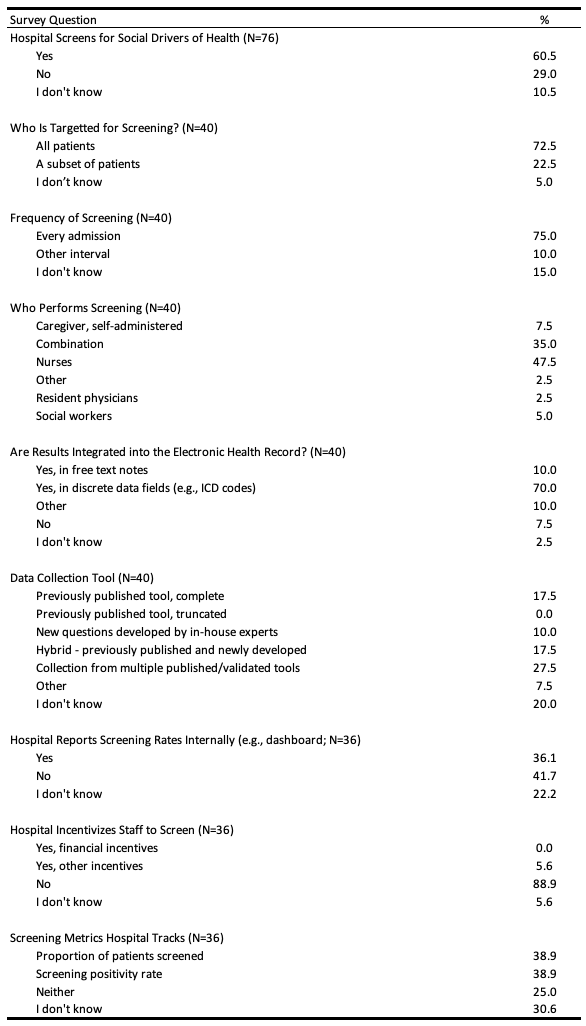
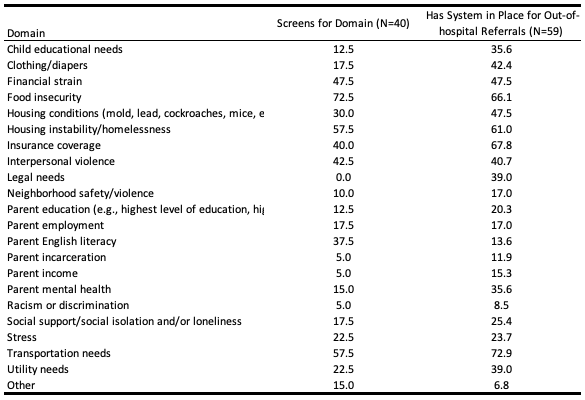
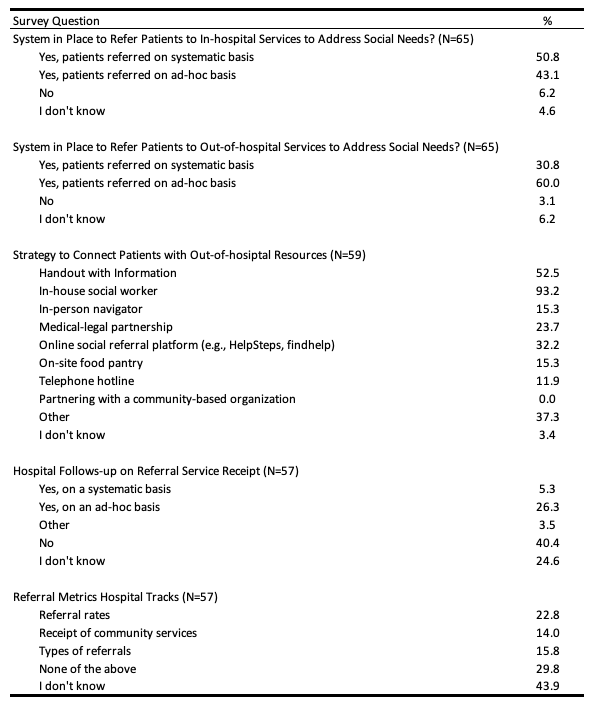
Results: We received a response to at least one question from 79 hospitals (82.3%) and complete responses from 60 hospitals (62.5%). Sixty percent of hospitals perform some form of SDOH screening, with 72.5% of those screening targeting all patients and 75.0% screening patients on every admission. Data collection tools vary widely, with 17.5% using a previously published complete tool and 10.0% using new questions developed by in-house experts. Nurses most commonly screen patients (Table 1). Screening domains range from a low of 0% screening for legal needs to 57.5% screening for housing instability. Referral systems in place for domains range from a low of 6.8% for “other” needs to 72.9% for transportation needs (Table 2). 93.9% of hospitals have systems in place to refer patients to in-hospital social services and 90.8% have systems for out-of-hospital referrals. Strategies to connect patients with resources ranged from 0% partnering with community-based organizations to 93.2% referring to in-house social workers to make referrals (Table 3).
Conclusion(s): We found wide variation in SDOH screening and referral practices among pediatric hospitals. Policies that incentivize and support standardized SDOH screening and responses might reduce variation and promote more equitable practices among US hospitals.