Critical Care
Session: Critical Care 2
121 - Characterization of Urgent ICU Consultations in the The EPOCH Randomized Clinical Trial
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 121
Publication Number: 121.2750
Publication Number: 121.2750

Andrea E. Pisesky, MBBS
Clinical Fellow
The Hospital for Sick Children
Toronto, Ontario, Canada
Presenting Author(s)
Background: Urgent PICU consultation – by rapid-response or other ICU team – may include reassurance, resuscitation, or redirection of care, and patients may remain on the ward, or be transferred to high dependency units or ICU. The EPOCH cluster RCT evaluated urgent ICU consultations for 18 months in 21 hospitals. Urgent ICU consultation outcomes have not been reported.
Objective: To describe the outcomes of urgent ICU consultations.
Design/Methods: We performed a secondary analysis of patients in the EPOCH trial who had one or more urgent ICU consultations. We defined a care episode as consecutive ICU consultations until either an ICU admission or at least two weeks without an ICU consultation. Outcomes were the disposition of patients after each consultation, the provision of resuscitation interventions for patients remaining on the wards and the occurrence of late ICU admission for patients admitted to ICU.
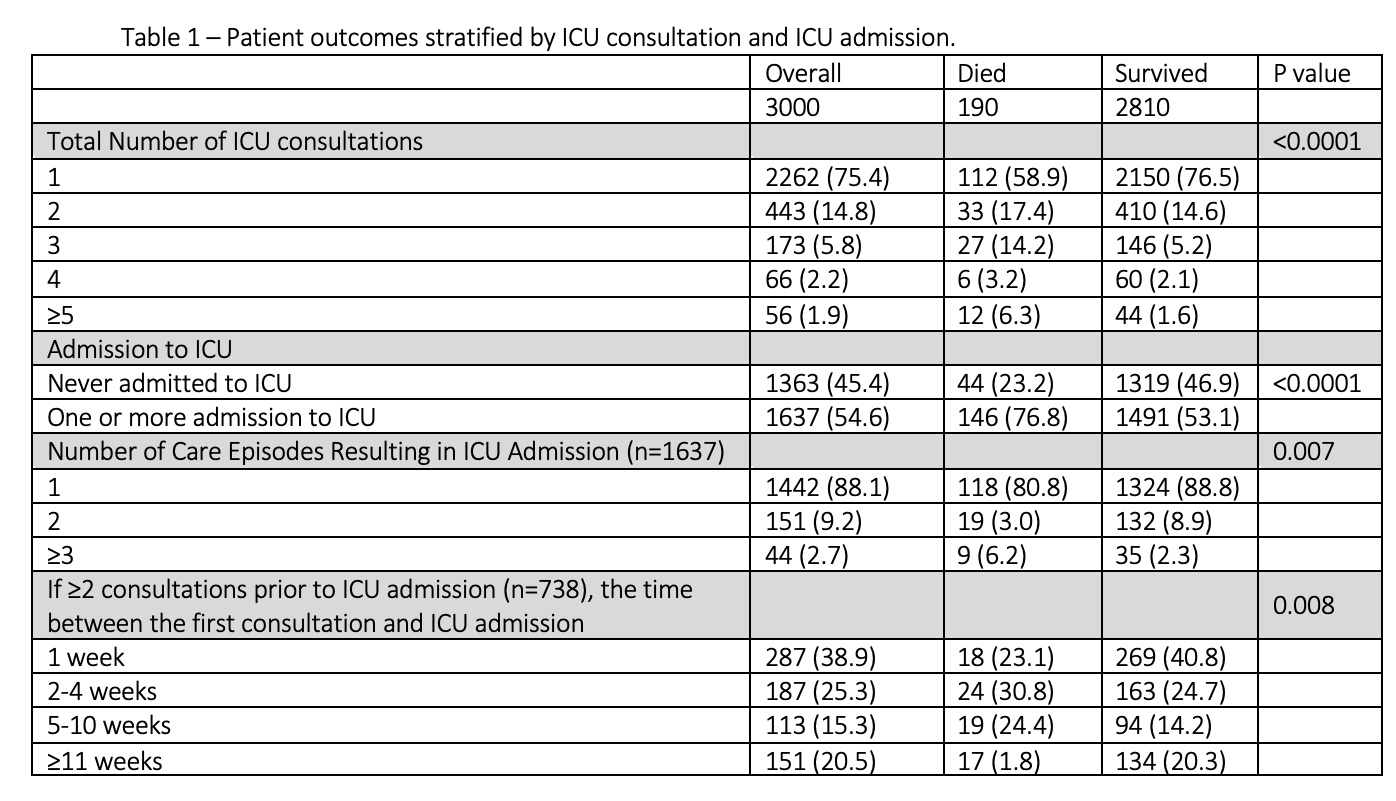
Results: 4288 individual ICU consultations comprised 3625 care episodes in 3000 patients of median (IQR) age of 25 (5-99) months at the last care episode. There were 12 (IQR 8, 23) consultations per 1000 discharges; 443 (14.8%) patients had two, 173 (5.8%) had three and 122 (4.1%) had 4 or more consultations.
The first consultation of the last care episode resulted in 1477 (49%) ICU admissions, with a median (IQR) lCU stay of 4 (2-8) days, and 3 (0.1%) in-consultation deaths. Late ICU admissions occurred in 269 (18%). Among the 1500 (50.0%) who remained on the ward 20 (0.7%) were transferred to another non-ICU location and the resuscitation interventions provided to 120 (7.9%) patient: included fluid boluses in 75 (4.9%), respiratory support in 44 (2.9%) and DNR orders in 12 (0.8%). During the 401 last care episodes with repeated ICU consultations, there were 218 ICU admissions, of which 39 (18%) were late ICU admissions (p=0.91). Death occurred in 190 (6.3%) patients during their hospital admission, of whom 82 (43.2%) died outside of the ICU. Patients who died were more likely to have multiple ICU consultations and any ICU admission (p < 0.0001).
Conclusion(s): Urgent consultation to for PICU expertise occurred in about one per 100 hospitalized patients and led to ICU admission in half of consultations. Patients with recurrent consultation and resuscitation had an increased risk of hospital mortality and future deterioration, although were not found to be at increased risk of urgent ICU admission on their second or subsequent consultation suggesting consulting teams are judging each consultation independently.