Neonatology
Session: Neonatal Infectious Diseases/Immunology 3
630 - Urinary tract infections in preterm infants: Review in two Canadian tertiary centres
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 630
Publication Number: 630.601
Publication Number: 630.601

Bao-Nghi Nguyen, MD (she/her/hers)
Research Assistant
University of Alberta Faculty of Medicine and Dentistry
Markham, Ontario, Canada
Presenting Author(s)
Background: Urinary tract infections (UTI) in premature infants are commonly seen in the neonatal intensive care unit (NICU). The reported prevalence of UTI in this population ranges from 1.9-12.2% due to the lack of standardized criteria for UTI among infants less than two months of age. Enterococcus and Enterobacteriaceae are well known to cause UTI and their resistance pattern has been reported to be rising in the neonatal nosocomial infections worldwide.
Objective: To describe the epidemiology, microbiology, and antimicrobial treatment for UTI in premature infants based on different diagnostic criteria.
Design/Methods: This retrospective study (2019-2022) included infants born at < 33 weeks of gestational age (GA) with positive urine cultures and ≥5 days of antimicrobials treatment. We collected data from two tertiary level NICUs in Canada, including demographics, microbial susceptibility patterns, urinalysis and imaging results, and antibiotic treatment.
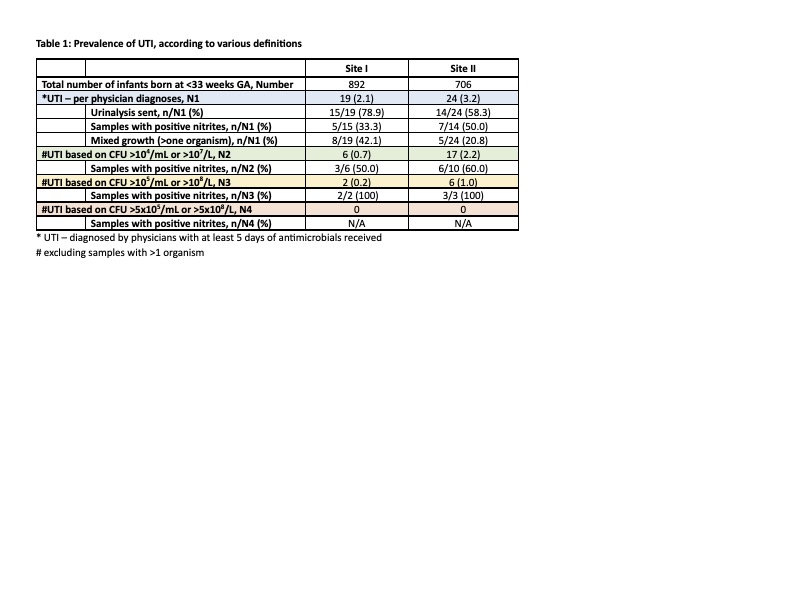
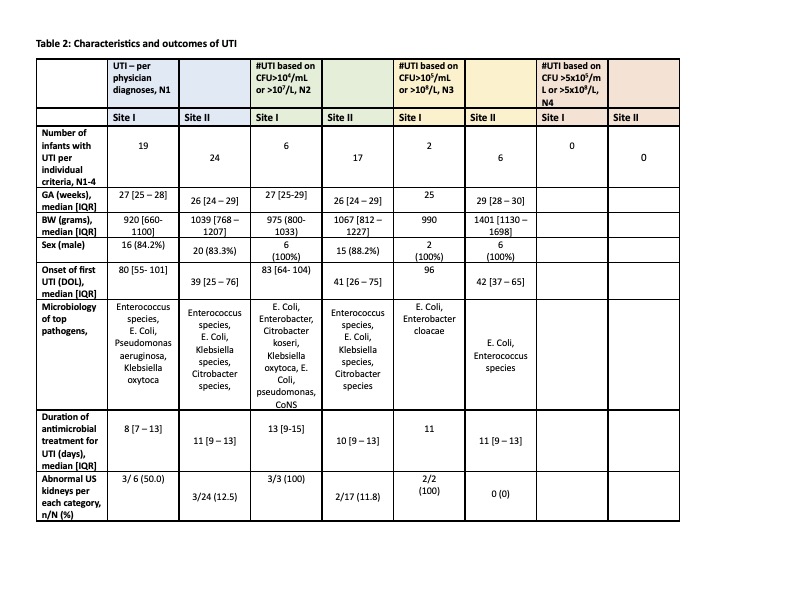
Results: We identified 43 infants managed as UTI based on physicians’ discretions. The median GA at birth was 26-27 weeks, while the median onset of first UTI ranged 39-80 days, with male predominance [Table 2]. Mixed growth of organisms constituted 21-42% of cases of UTI [Table 1].
Among UTI cases with only single growth organism, we found 53.5% and 18.6% cases fulfilled UTI diagnostic criteria based on the concentration of colony forming units (CFU) of >104/mL or >107/L and >105/mL or >108/L, respectively [Table 1].
Of these cases, 67.4% of infants had urinalysis sent with the culture, and the higher the concentration of CFU, the more likely the samples showed positive nitrites on urinalysis, with 100% correlation among those with CFU >105/mL or >108/L. [Table 1]
The most common pathogens were Enterococcus species, E.Coli, Klebsiella species, Citrobacter species and Enterobacter cloacae complex [Table 2]. Among gram negative bacilli (E. Coli and Klebsiella species), greater than 42-80% were resistant to 3rd generation cephalosporins (3GC). We did not identify any vancomycin-resistant Enterococcus strains.
Median duration of antimicrobial treatment ranged from 8-13 days, depending on the diagnostic criteria applied. At least 10% of infants with UTI showed abnormalities on kidney ultrasound [Table 2].
Conclusion(s): There exists a large variation in UTI prevalence according to different diagnostic criteria. Abnormal urinalysis with presence of nitrites were frequently associated with UTI of high CFU count. High resistance to 3GC among gram negative bacilli was concerning and carried an impact on the appropriate empirical treatment choice.