Neonatology
Session: Neo-Perinatal Health Care Delivery 1: Epidemiology/Health Services Research
317 - Impact of Infants 22 Weeks’ Gestation on U.S. Neonatal ICUs, 2008-2021
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 317
Publication Number: 317.1093
Publication Number: 317.1093
Matthew Rysavy, MD, PhD (he/him/his)
Assistant Professor / Director of Learning Healthcare
UTHealth Houston
Houston, Texas, United States
Presenting Author(s)
Background: The provision of intensive care for infants born at 22 weeks’ gestation has increased during the past decade. The impact of this change on hospitals is unknown.
Objective: To characterize recent trends in neonatal intensive care unit (NICU) resource utilization for infants born at 22 weeks’ gestation compared to other NICU-admitted infants.
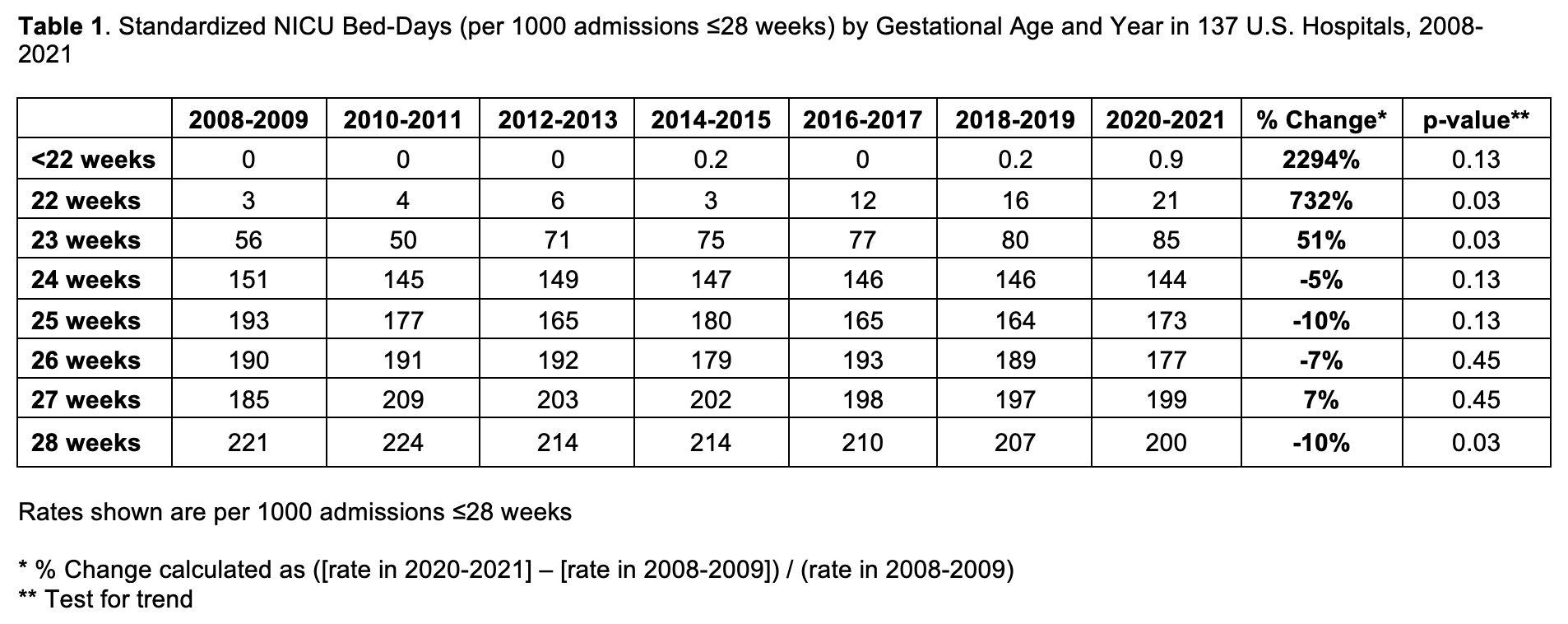
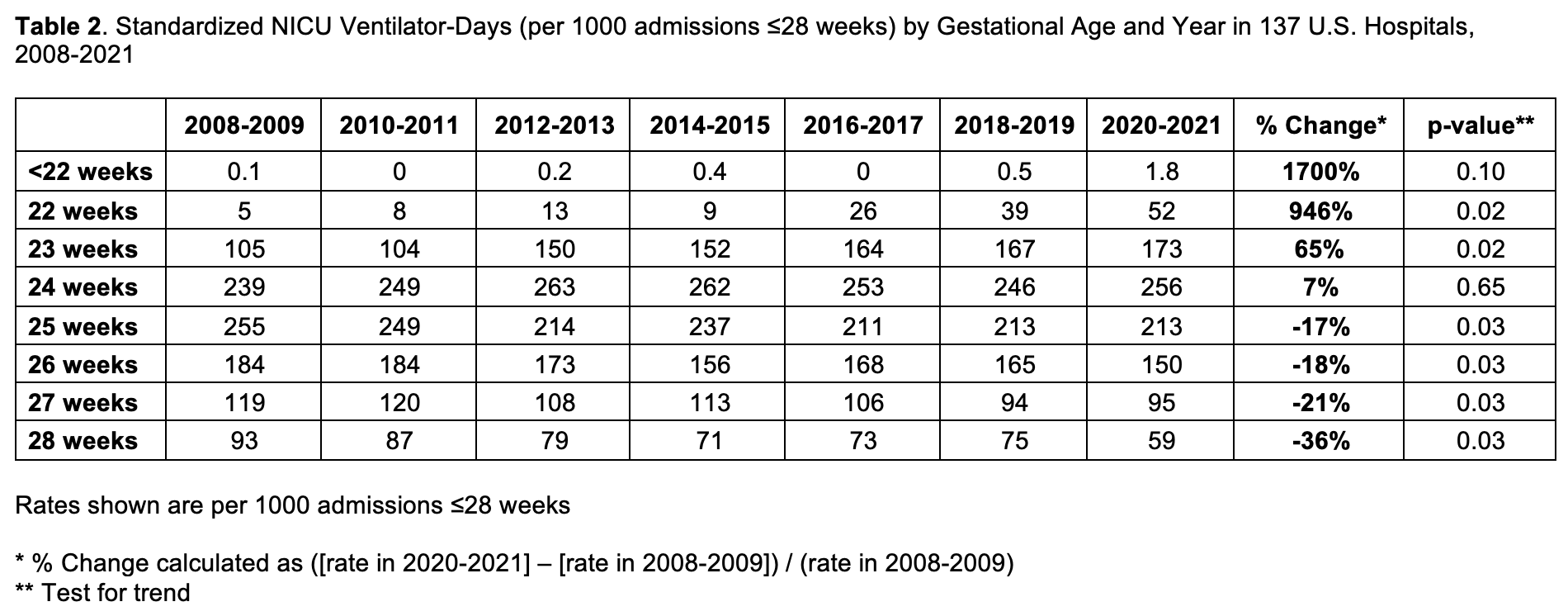
Design/Methods: We used annual cross-sections of a national clinical dataset with data from 137 U.S. NICUs in 29 U.S. states from 2008 through 2021 to characterize recent trends in neonatal intensive care unit (NICU) resource utilization for infants born at 22 weeks’ gestation compared to other extremely preterm infants (≤28 weeks’ gestation). Measures of resource utilization included NICU admissions, NICU bed-days, and ventilator-days.
Results: Of 825,112 infants admitted to 137 NICUs 2008 to 2021, 60,944 were extremely preterm and 872 were 22 weeks’ gestation. NICU admissions at 22 weeks’ gestation increased from 5.7/1000 extremely preterm admissions in 2008-2009 to 27.8/1000 extremely preterm admissions in 2020-2021 (Figure). This corresponded to an increase from 2.5/1000 to 20.8/1000 extremely preterm NICU bed-days (Table 1) and 5.0/1000 to 52.3/1000 extremely preterm ventilator-days, respectively (Table 2). The proportion of NICUs admitting infants born at 22 weeks increased from 23% to 46%. Increases in resource use were also observed for infants born at < 22 and 23 weeks. In 2020-2021, infants ≤23 weeks contributed 1 in 117 of all NICU admissions, 1 in 34 of all NICU bed-days, and 1 in 6 of all NICU ventilator-days.
Conclusion(s): From 2008 to 2021, a substantial and increasing share of resources in U.S. NICUs was allocated to infants born at 22 weeks’ gestation.
.png)