Neonatology
Session: Neonatal Infectious Diseases/Immunology 2
602 - Antimicrobial Stewardship Programs in Neonates: A Systematic Review and Meta-Analysis
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 602
Publication Number: 602.611
Publication Number: 602.611
.jpg)
Dwayne D. Mascarenhas, MD, DM (he/him/his)
Clinical Fellow
University of Toronto
Toronto, Ontario, Canada
Presenting Author(s)
Background: Neonatal sepsis constitutes a significant challenge in healthcare, both in terms of mortality and morbidity, thereby accentuating the increased need for effective antimicrobial stewardship programs (ASP) considering specific needs of neonates.
Objective: Our objective was to systematically review the multifaceted components in neonatal ASPs, their impact on clinical outcomes, cost-effectiveness, antimicrobial resistance, and program sustainability.
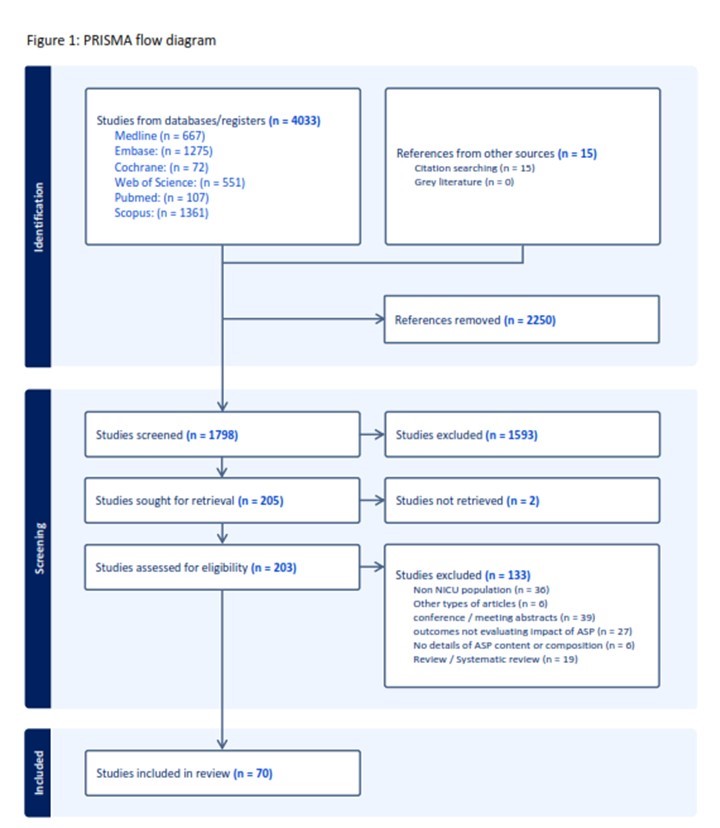
Design/Methods: We searched PubMed, Medline, Embase, Cochrane CENTRAL, Web of Science, and SCOPUS till May 22, 2023, for studies reporting the components and impact of neonatal ASPs. The PRISMA guidelines for systematic reviews were applied. We used the Newcastle-Ottawa scale to assess risk of bias and GRADE assessment for certainty of evidence. We estimated the pooled values for risk difference (RD) or mean difference (MD) between post-ASP (index) and pre-ASP (reference) groups using the random-effects model. Our review was registered with PROSPERO (CRD42023428258).
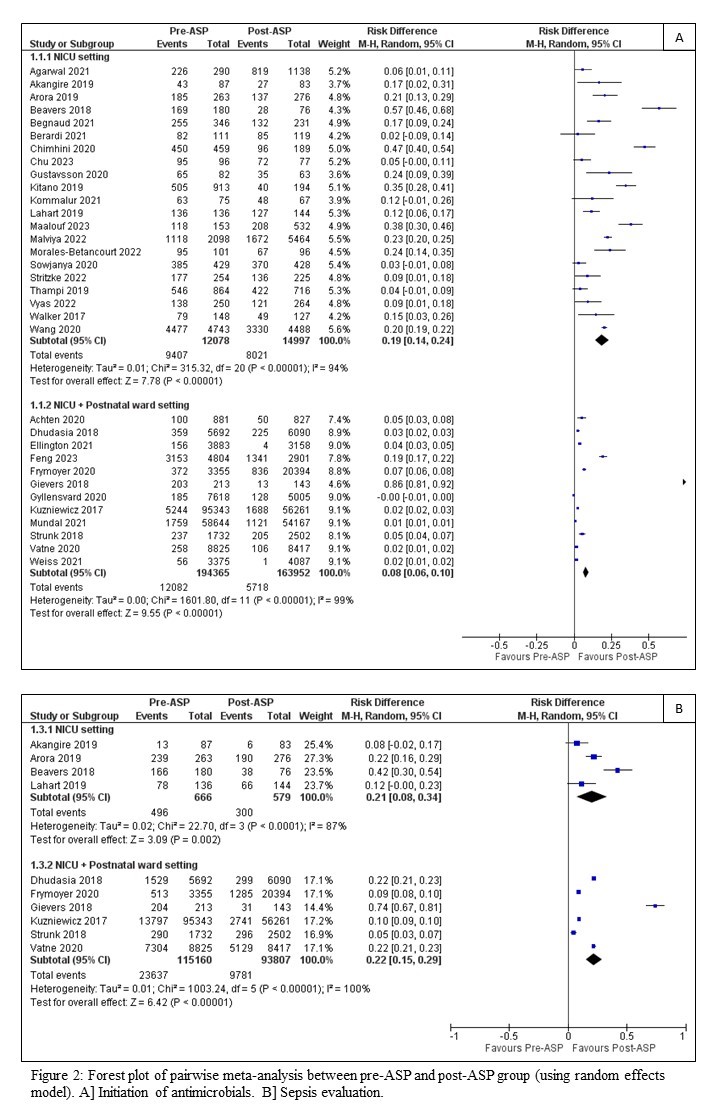
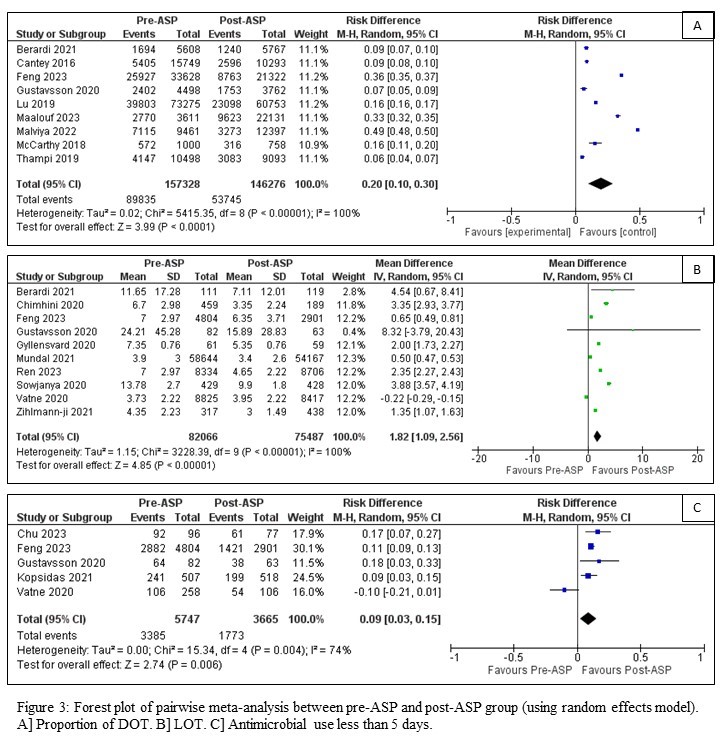
Results: Of the 4,048 studies retrieved, 70 studies (44 cohort and 26 observational studies), which enrolled >350,000 neonates met the inclusion criteria. Moderate certainty evidence suggests a significant reduction in antimicrobial initiation in NICU (pooled RD 19%; 95% CI 14-24%; 21 studies, 27,075 infants) and combined NICU and postnatal ward setting (pooled RD 8%; 95% CI 6-10%; 12 studies, 358,317 infants), proportion of days of therapy (pooled RD 20%; 95% CI 10-30%; 9 studies, 303,604 infants), length of therapy (pooled RD 1·82 days; 95% CI 1·09-2·56 days; 10 studies, 157,553 infants), and use of antimicrobials less than five days (pooled RD 9%; 95% CI 3-15%; 5 studies, 9,412 infants). Low certainty evidence suggests a reduction in economic burden and drug resistance, favorable sustainability metrices, without an increase in sepsis-related mortality or re-initiation of antimicrobials.
Conclusion(s): Moderate-to-low certainty evidence suggest that neonatal ASP interventions are associated with reduction in initiation and duration of antimicrobial treatment across NICU and postnatal settings, without an increase in adverse events.