Neonatology
Session: Neonatal Infectious Diseases/Immunology 1
594 - Placental Small Extracellular Vesicles (sEVs) promoted cell viability and attenuates proinflammatory cytokines expression by Lipopolysaccharide induced (LPS) mononuclear cells injury
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 594
Publication Number: 594.609
Publication Number: 594.609

Ranga Prasanth Thiruvenkataramani, MD (he/him/his)
Assistant Professor
Michigan State University College of Human Medicine
Lansing, Michigan, United States
Presenting Author(s)
Background: Sepsis is a risk factor for increasing neonatal morbidity and mortality, acute lung injury and chronic lung disease. Stem cell therapy alleviates acute lung injury mostly via paracrine effects and minimally via local engraftment. The paracrine effects are exerted through Mesenchymal stem cells (MSCs) derived Extracellular vesicles (EVs) which play a critical role in immune system modulation and tissue regeneration. Small EVs contain a cargo of mRNA, miRNA and protein. We previously have shown that Cord blood Plasma (CBP), Wharton jelly (WJ), and placental (PL) MSCs derived sEVs prevent cytotoxic effects in E. Coli lipopolysaccharide (LPS) on lung alveolar epithelial cells
Objective: To determine the effects of CB, WJ- and PL-MSCs-derived sEVs on cell viability and proinflammatory cytokines from monocytes cells after LPS treatment
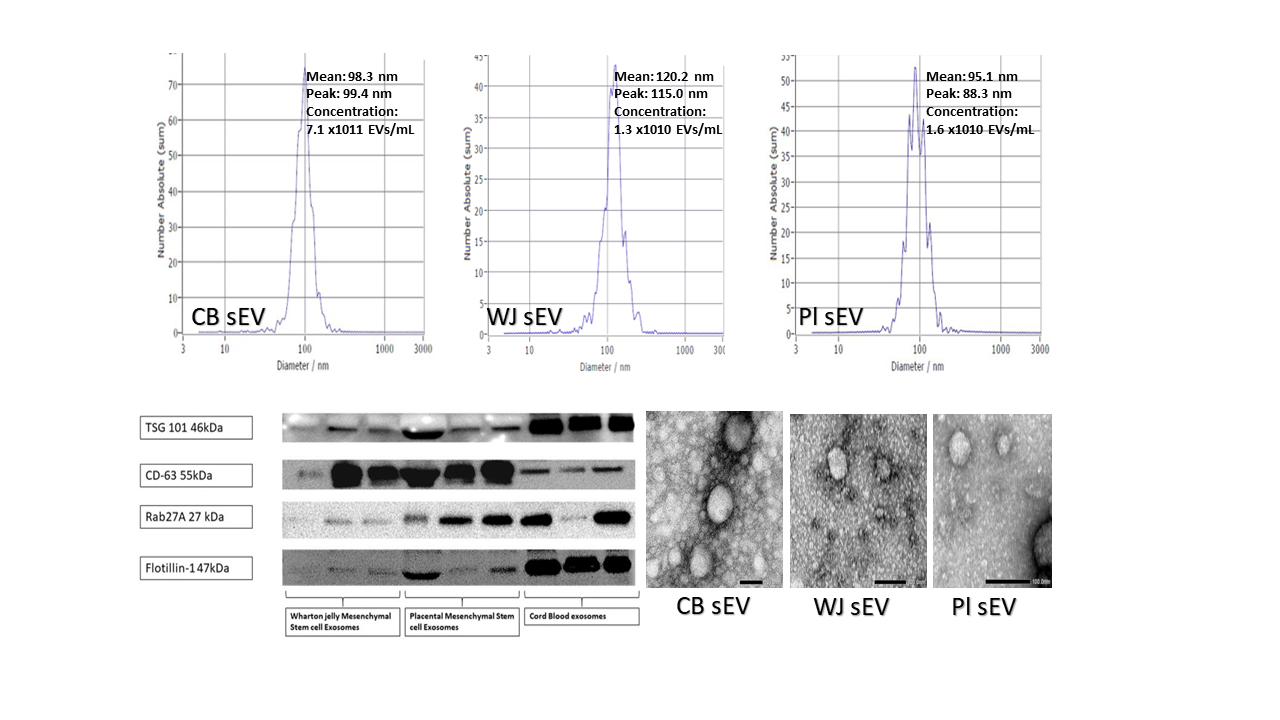
Design/Methods: After obtaining maternal consent, CB and placentas were collected from healthy full-term pregnancies. sEVs were collected by ultrafiltration from Pl- and WJ- MSCs conditioned media and CBP. sEVs were characterized based on Nanoparticle tracking analysis (NTA), Transmission electron microscopy (TEM), and western blotting techniques. The protein concentration of the isolated sEVs was used as a measure for treatment. Monocyte THP-1 cells were cultured and exposed to LPS treatment in the presence or absence of sEVs for 72 hrs. Cell viability was measured using CellTiter-Glo 2.0 chemiluminescence-based assay. THP-1 cells were incubated for 24hr +/- pl and CBP sEVs then 24hr +/- LPS. Supernatant media was collected, and Interleukin (IL)-6 and IL-8 cytokines were measured by ELISA technique. Statistical analysis was done by ANOVA
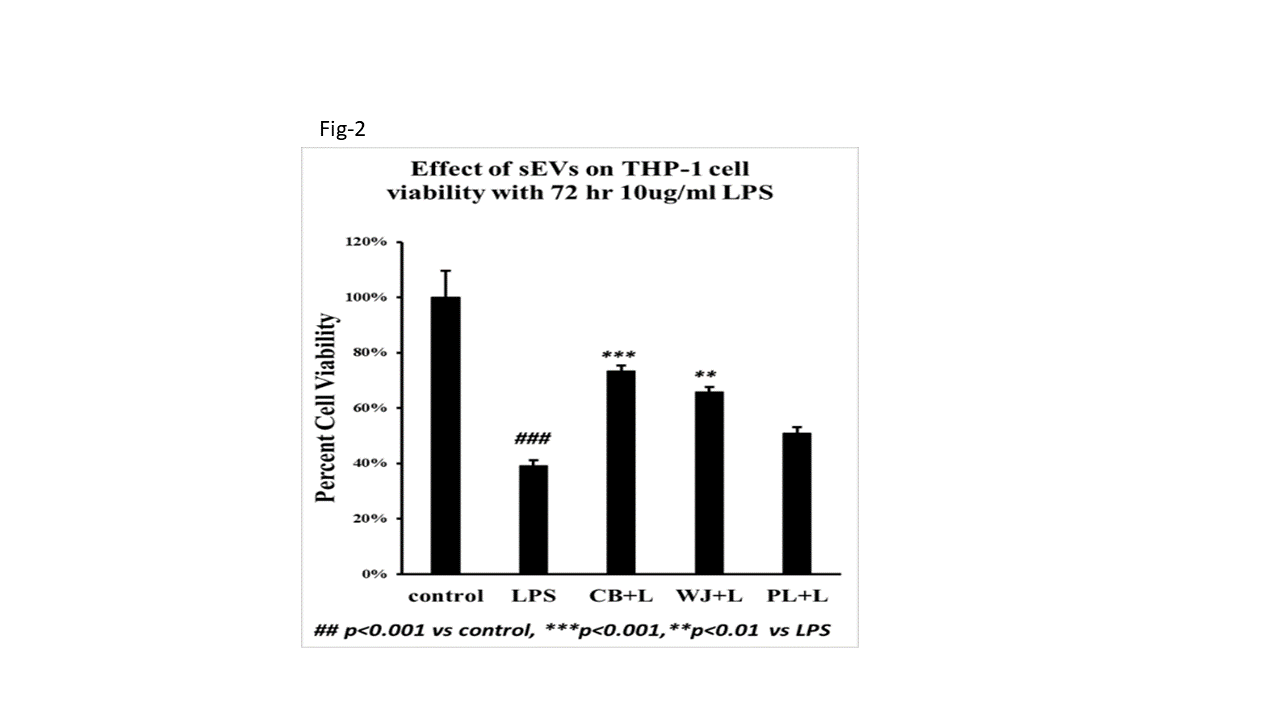
Results: The characteristics of the isolated sEVs are shown in Fig-1. LPS significantly reduced THP-1 cell viability. The presence of CB or WJ sEVs significantly increased cell viability compared with controls (Fig-2). Cells treated with PL sEVs showed increasing cell viability but did not reach statistical significance. LPS-treated cells showed a significant increase in IL-6 and IL-8. CB-, WJ- and PL- sEVs had a significant decrease in LPS-induced release of IL-6, whereas WJ sEVs decreased IL-8 but CBP and Pl-EVs increased IL-8 compared with the corresponding controls (Fig-3)
Conclusion(s): CB-, PL- and WJ-derived sEVs increased viability and decreased the release of pro-inflammatory cytokines from monocytes in response to LPS treatment. This suggests that placental sEVs can modulate the immune response, decrease inflammation, and prevent end-organ damage in neonates with sepsis