Neonatology
Session: Neonatal Infectious Diseases/Immunology 3
627 - Risk Factors and Prescribing Practices Among Preterm Infants with Urosepsis
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 627
Publication Number: 627.613
Publication Number: 627.613

Mohammed Alnajjar, MD, MSc (he/him/his)
Neonatal House Medical officer
Health Science Centre, Winnipeg
Winnipeg, Manitoba, Canada
Presenting Author(s)
Background: Urinary tract infections (UTI) affect approximately 25% of preterm infants. Risk factors for occurrence of UTI have been well described; however, little is known about the occurrence of urosepsis (positive urine and blood cultures with the same organism).
Objective: To describe the risk factors and prescribing practices among preterm infants with urosepsis.
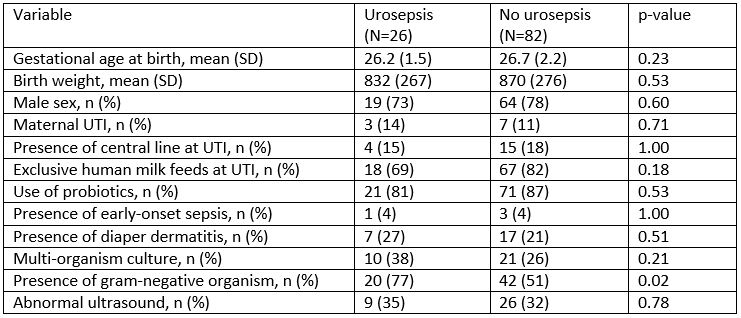
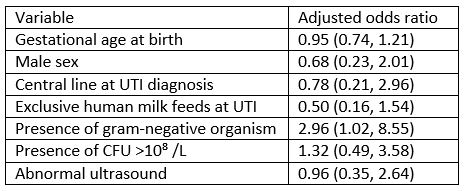
Design/Methods: Retrospective cohort study of all infants < 35 weeks gestational age (GA) admitted to the NICU over a 6-year period with UTI, defined as positive urine culture and antimicrobial treatment for 5 days. Key demographic data and details of each UTI episode including presenting symptoms, pathogen, type and duration of antimicrobial therapy, were collected. Ultrasounds (US) were reviewed for the presence of structural abnormalities. The cohort was divided into 2 groups: infants with urosepsis, and those with UTI only. Demographic and clinical characteristics were compared between the two groups. Logistic regression (LR) was performed to identify risk factors for urosepsis after adjusting for GA, male sex, and presence of a gram-negative organism.
Results: Of the 108 infants with UTI, 26 (24%) developed urosepsis. The most common pathogens were E. faecalis (n=45, 42%), Klebsiella species (n=20, 19%) and E. coli (n=18, 17%). Twelve (11%) of patients had pyelectasis or hydronephrosis on US. Baseline characteristics were not different between the two groups (Table 1). The presence of a gram-negative organism was significantly associated with the development of urosepsis (77% vs. 51%, p=0.02); this was maintained on LR (adjusted OR 2.96 [95% CI 1.02, 8.55]). Bacterial load (colony forming units [CFU]/L) was not associated with urosepsis development, but infants with gram-negative infection were more likely to have >10⁸ CFU/L than < 10⁸ CFU/L (69% vs. 48%, p=0.03). Patients with urosepsis received longer antimicrobial duration (14 6 vs. 8 2 days, p< 0.01). There was variability in prescribing practices; most infants received ampicillin (n=45, 42%). Infants with urosepsis were more likely to receive broad-spectrum antibiotics (81% vs. 45%, p< 0.01).
Conclusion(s): Urosepsis is a common occurrence among infants with UTI, and affected patients receive longer duration and more frequent broad-spectrum antimicrobial therapy. These data suggest that when UTI is suspected, blood culture should be collected to rule out concomitant bacteremia. Empiric antibiotic therapy should include gram-negative coverage. Antimicrobial stewardship may address variability in antibiotic choice and duration.