Neonatology
Session: Neonatal Follow-up 3
533 - Concordance with Neonatal Intensive Care Unit (NICU) Follow-Up Recommendations and Post-Discharge Health Outcomes
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 533
Publication Number: 533.2742
Publication Number: 533.2742

Anjana Bhami Shenoy, MBBS (she/her/hers)
Research Coordinator II
University of Massachusetts Chan Medical School
Worcester, Massachusetts, United States
Presenting Author(s)
Background: Studies in adults have shown that concordance with regular outpatient follow-up visits reduces rehospitalizations in patients with a history of stroke or schizophrenia. In pediatric patients with chronic disease, limited data is available on the association between concordance with recommended follow-up guidelines and rates of rehospitalization, emergency department visits, or other health outcomes. Some studies in children with cystic fibrosis show upward trends in anthropometric data in those who are concordant with follow-up, but research on readmission rates and other outpatient health indicators following discharge from the neonatal intensive care unit (NICU) is lacking.
Objective: The objective of this study was to assess the association of concordance with recommended follow-up visits at the UMass Memorial Medical Center (UMMMC) Center for Healthy Infant Development (CHILD) with post-discharge health outcomes.
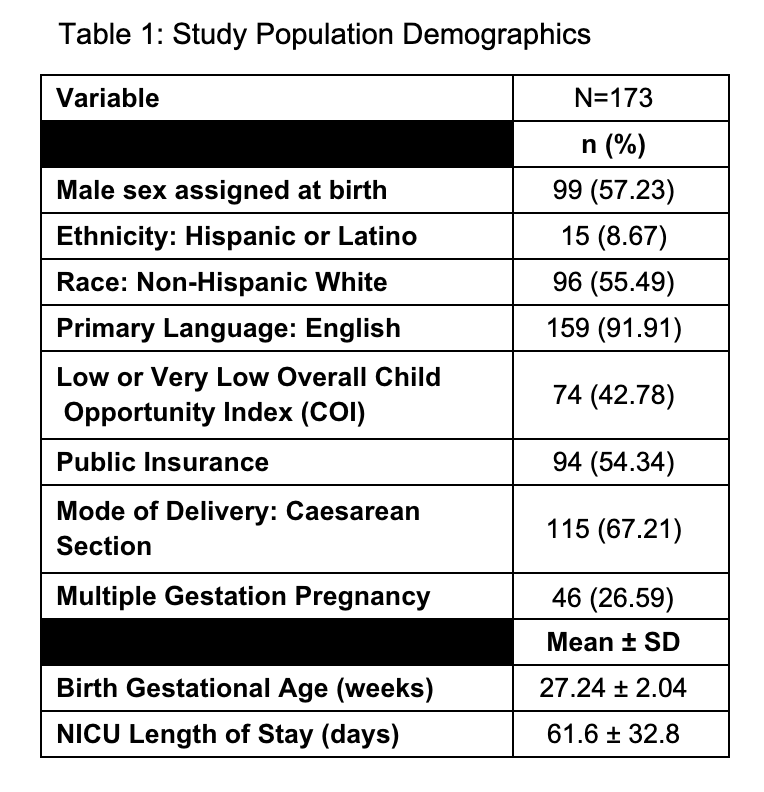
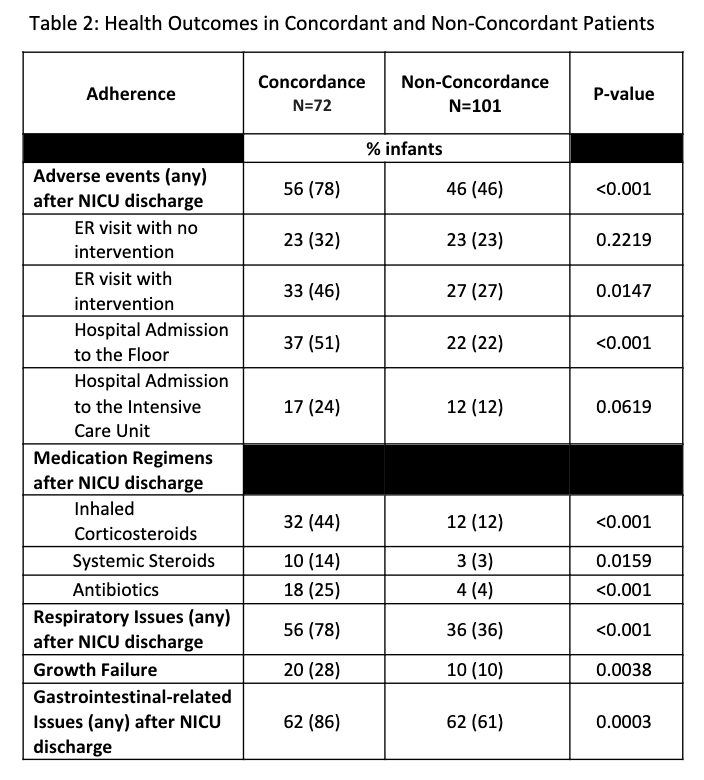
Design/Methods: This was a single-center, retrospective cohort study of all infants discharged from the UMass Memorial Medical Center (UMMMC) NICU born less than 30 weeks gestational age who attended at least one visit in CHILD between October 2016 and April 2021. Concordance was defined as attendance at all recommended visits during the first-year post-discharge (quarterly visits if not on home oxygen, monthly visits if on home oxygen). Post-discharge respiratory status, growth, feeding, medications, and adverse events were abstracted from the infant’s electronic medical record. Adverse events were defined as any emergency room (ER) visit or readmission following discharge from the NICU. Post-pandemic was defined as birth after March 2020. Bivariate and multivariate measures of association were calculated between concordance and a variety of outcomes.
Results: A total of 173 infants (57% male) had at least one visit in CHILD during the study period, of which 72 (42%) were concordant with follow-up guidelines. Concordance with recommended preventative clinic schedule was significantly associated with decreased adverse events after adjustment for the pandemic. Interestingly, patients with higher concordance had more respiratory issues, growth failure, and gastrointestinal related issues and were more likely to be on maintenance outpatient medication regimens.
Conclusion(s): This study found that concordance with recommended follow-up visit schedule improved health outcomes for former premature infants. Strategies to improve concordance should be investigated.
.png)
