Neonatology
Session: Neonatal Quality Improvement 1
382 - Implementation of A Cue-Based Feeding Protocol to Facilitate Safe Oral Feeding for Preterm Infants on CPAP
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 382
Publication Number: 382.2296
Publication Number: 382.2296

Melis Suner, MD (she/her/hers)
Fellow
Icahn School of Medicine at Mount Sinai
New York, New York, United States
Presenting Author(s)
Background: Continuous positive airway pressure(CPAP) effectively supports respiratory function and lung development in preterm infants. At a developmental stage when they approach readiness to oral feed, many preterm infants rely on CPAP.
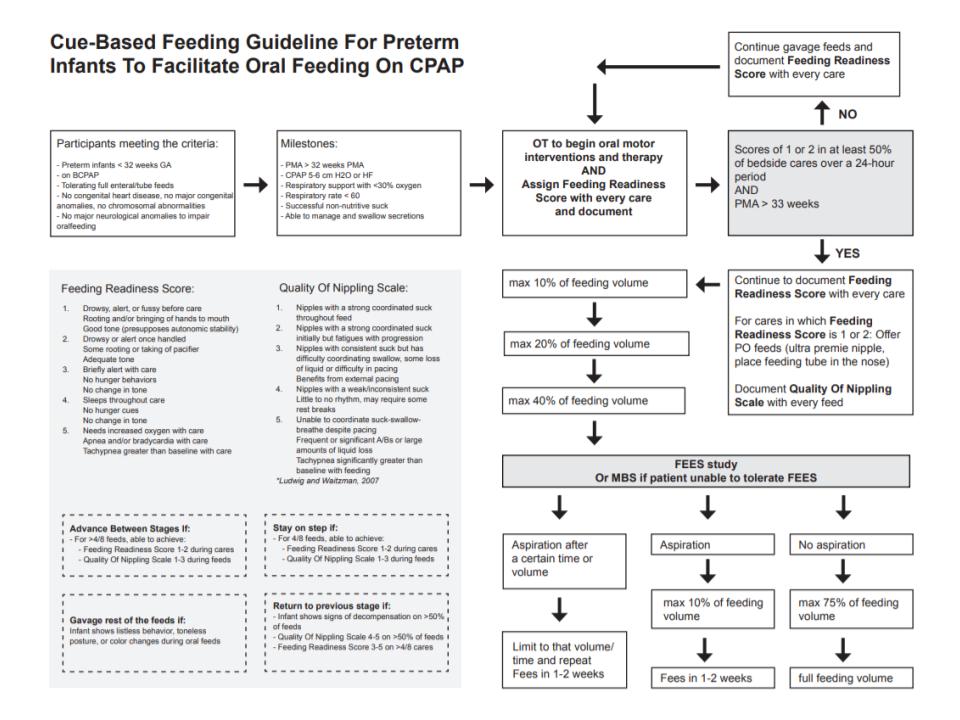
Objective: Implementation of a cue-based feeding program for safe initiation and advancement of oral feeds in preterm infants born before 32 weeks who remain on CPAP at the time when feeding skills emerge.
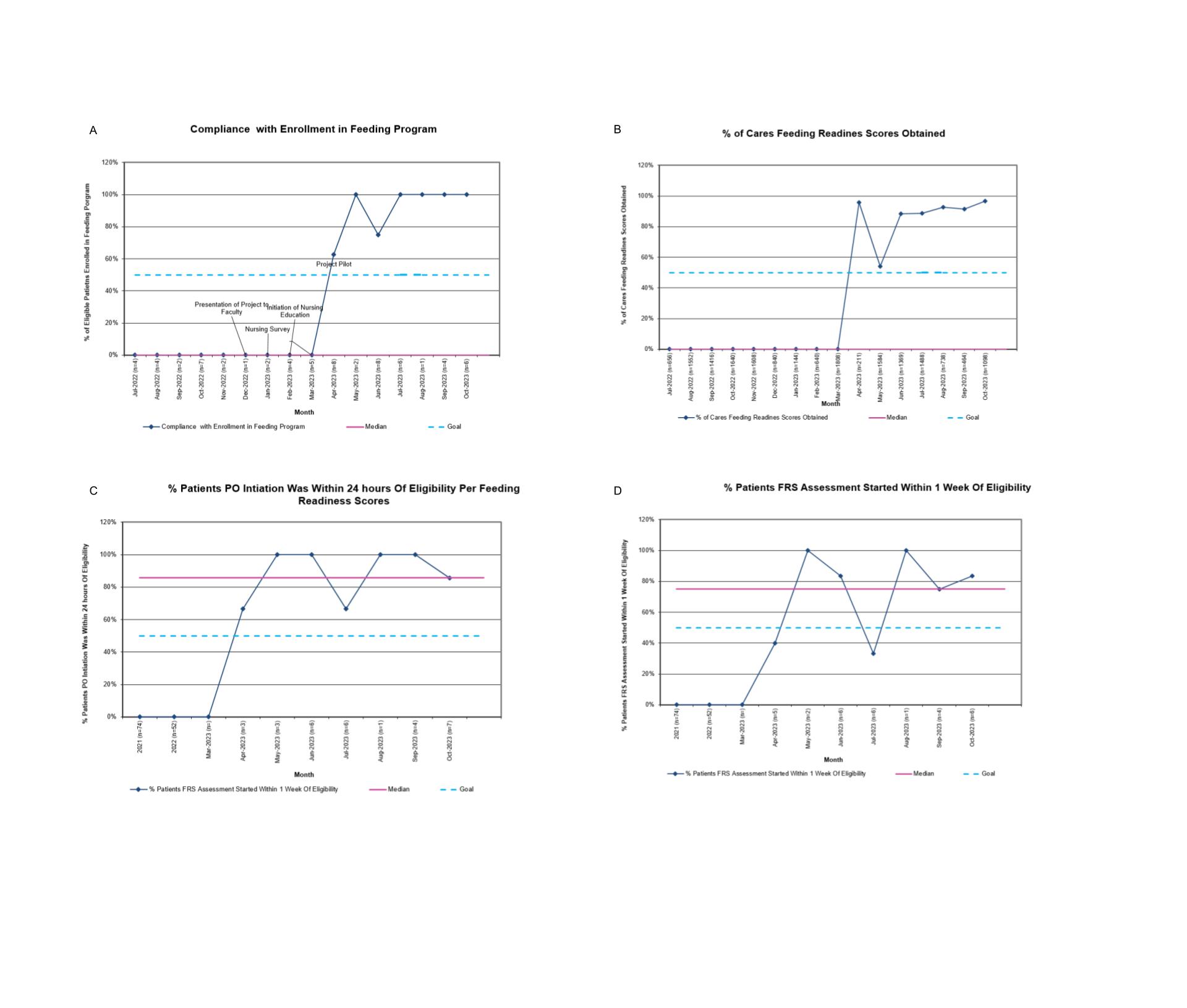
Design/Methods: A baseline chart audit was conducted to assess current practices. A survey was conducted to nurses to identify barriers to feed infants on CPAP.A multidisciplinary committee, including neonatologists, feeding and speech therapists, and nurses, reviewed existing literature. The committee designed a novel protocol to assess feeding readiness and initiate infant-driven oral feeds in ex-premature infants born before 32 weeks gestation who had reached 32 weeks post menstrual age and remained on CPAP.Nurses were educated on performing feeding readiness and quality of nipping assessments. EMR flowsheets were modified to facilitate documentation of these data points.A process for identifying eligible infants and signaling readiness for assessment was established. Compliance with enrollment and protocol elements was tracked using U-charts over time.For infants progressing on PO feeds while on CPAP, safety was assessed with Flexible Endoscopic Evaluation of Swallow(FEES).
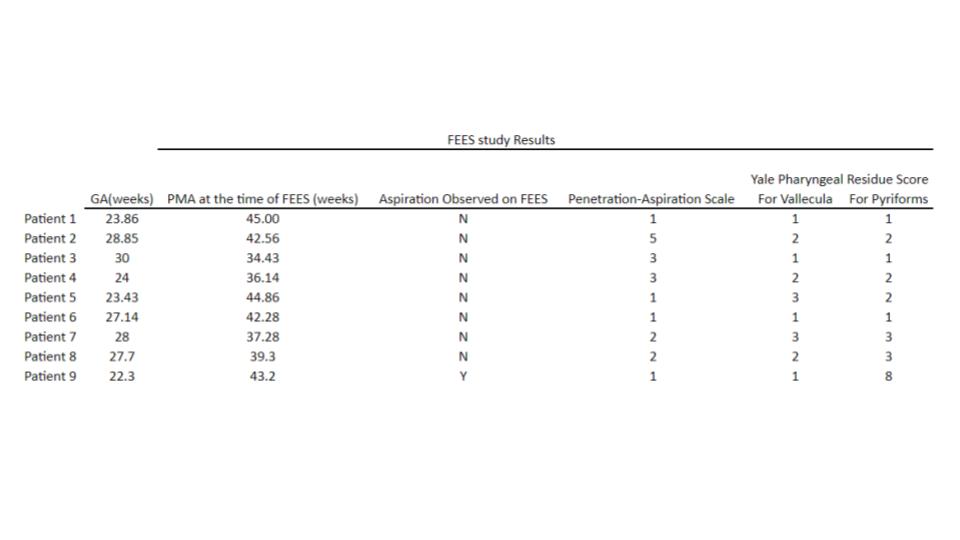
Results: The baseline chart audit covered the period from October 1, 2020, to September 30, 2022, and included 133 patients.Only 6 out of the 133 patients began oral feeds while on CPAP. A survey was completed by 64 nurses, with 50% indicating the belief that transitioning a CPAP-supported infant to high or low flow nasal cannula was necessary for oral feeds.Since initiating a program pilot in April 2023 and full roll-out in May 2023, 30 patients(86% of all eligible) were enrolled and underwent cue-based scoring.26 of 30 enrolled patients(86%) had their initial feeds on CPAP. Compliance with scoring, assessments, and timely/appropriate initiation of oral feeds were tracked over time and exceeds 70% across all domains.Nine patients underwent FEES while feeding on CPAP.In 8 cases, the Penetration-Aspiration Scale was < 6, indicating no observed aspiration.
Conclusion(s): This Quality Improvement initiative established a standardized approach to initiation and advancement of oral feeding based on an infant-driven cues for infants on CPAP.These preliminary results indicate that a cue-based approach to feeding on CPAP is possible and safe and outlines potential processes that can be utilized by other centers.