Health Equity/Social Determinants of Health
Session: Health Equity/Social Determinants of Health 2
442 - A Case Study: Proxy Use of Online Patient Portals on Behalf of Children at Federally Qualified Health Centers
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 442
Publication Number: 442.3
Publication Number: 442.3

Omolola E. Adepoju, PhD, MPH
Clinical Associate Professor
University of Houston College of Medicine
Houston, Texas, United States
Presenting Author(s)
Background: Proxy online health-information seeking is frequently exhibited in parent-child relationships. However, prior studies of pediatric patient portal use by parents have shown disparities in portal enrollment, activation, and usage. Few studies focused on portal usage in low-resourced populations and settings, such as Federally Qualified Health Centers (FQHCs). Because FQHCs are a major safety net, it is important to learn about the drivers of portal use in vulnerable populations receiving care in low-resource settings.
Objective: This study examined the proxy use of patient portals for children in a large Federally Qualified Health Centers (FQHC) network in Texas.
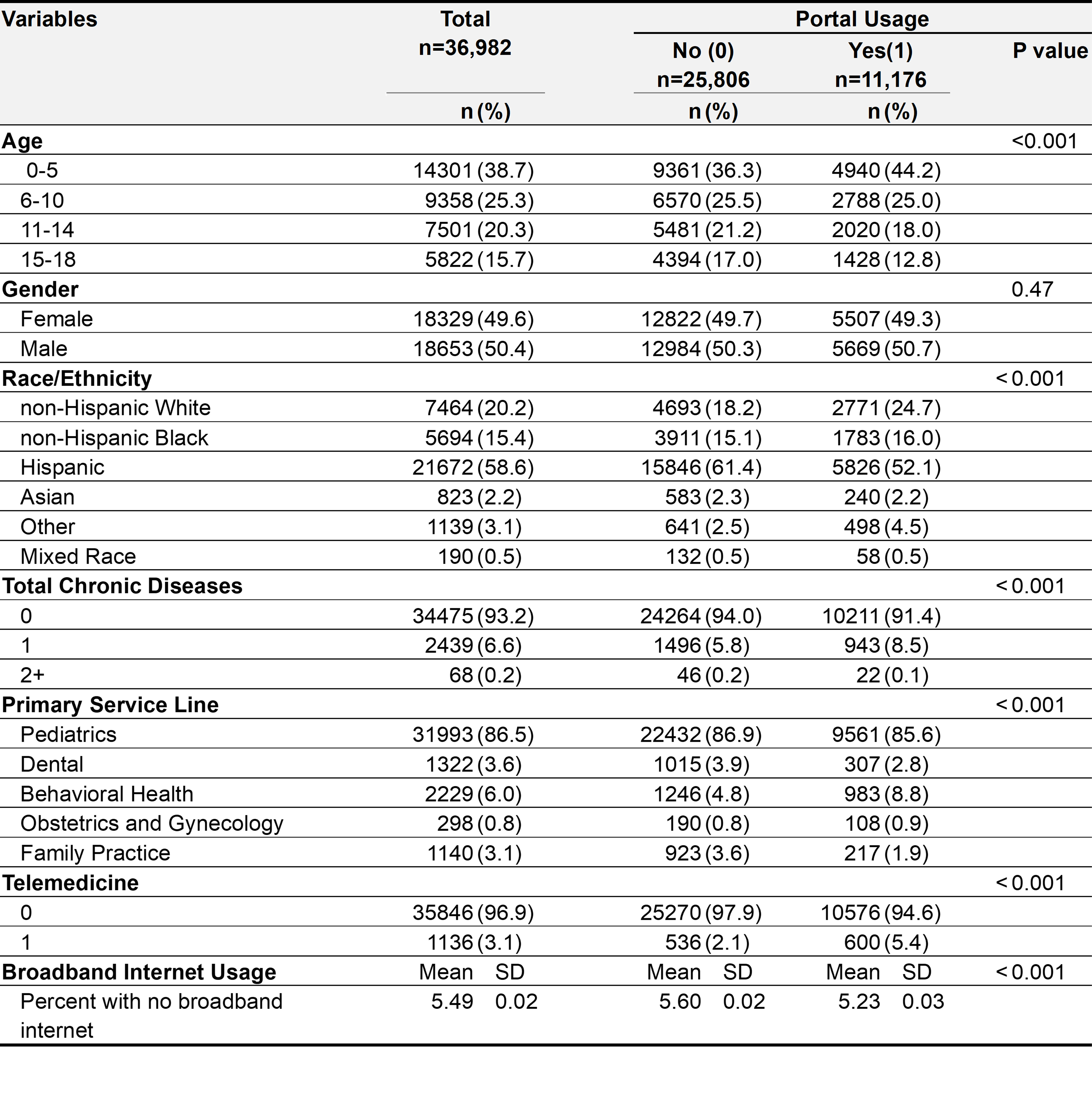
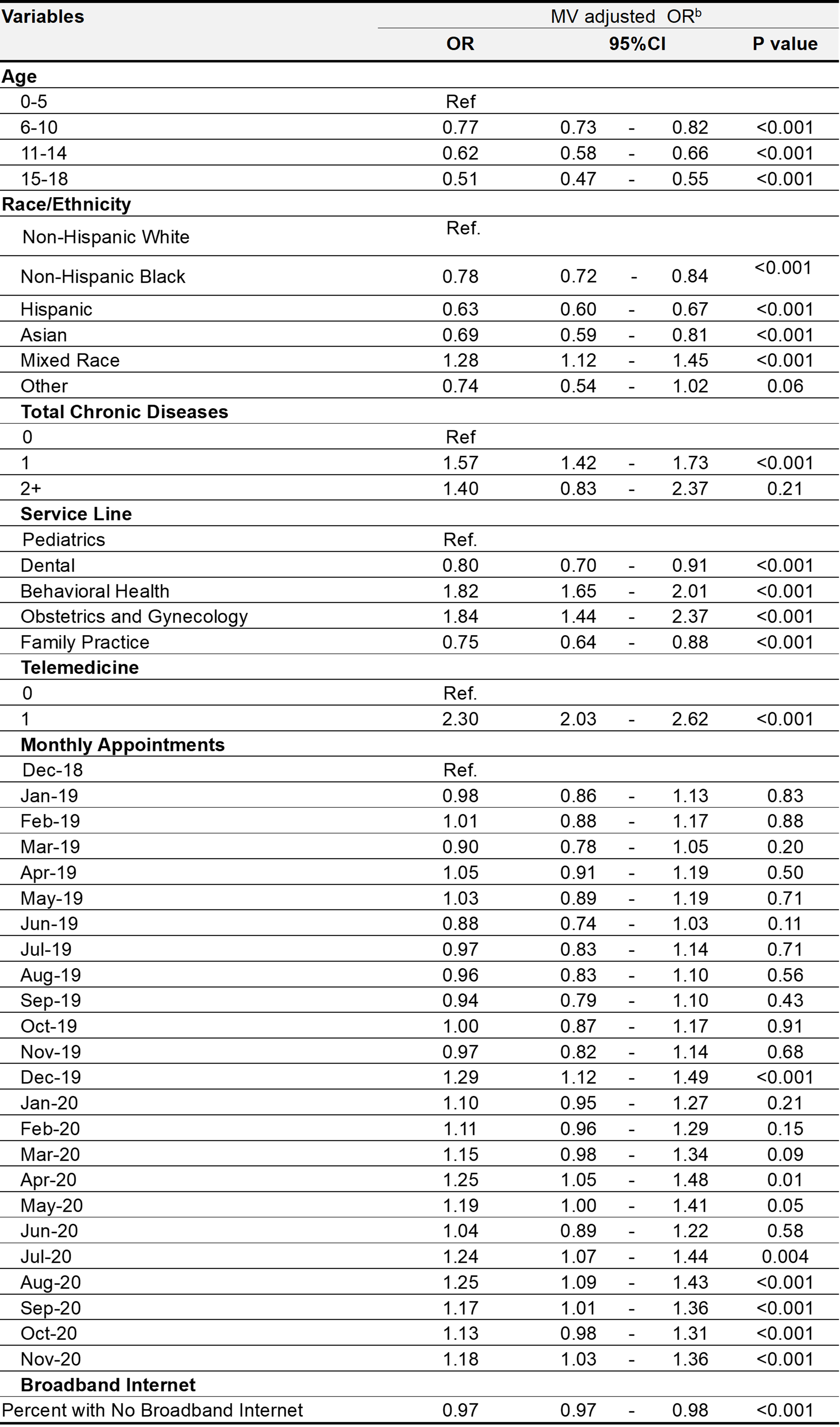
Design/Methods: We used de-identified individual-level data of patients, 0-18 years, who had 1+ visits between December 2018-November 2020. Logistic regression was used to examine patient-, clinic- and geographic-level factors associated with proxy portal usage.
Results: The proxy portal usage rate increased from 28% in the pre-pandemic months (November 2018-February 2020) to 34% in the pandemic months (March-Nov 2020). Compared to patients 0-5 years, patients aged 6 to 18 years had lower odds of portal usage (6-10 OR: 0.77, p< 0.001; 11-14 OR: 0.62, p< 0.001; 15-18 OR: 0.51, p< 0.001). Minoritized groups had significantly lower odds of portal usage when compared to their Non-Hispanic White counterparts (Non-Hispanic Black OR: 0.78, p< 0.001; Hispanic OR 0.63, p< 0.001; Asian OR: 0.69, p< 0.001). Having one chronic condition was associated with portal usage (OR: 1.57, p< 0.001); however, there were no significant differences in portal usage between those with none or multiple chronic conditions. Portal usage also varied by service lines, with obstetrics and gynecology (OR: 1.84, p< 0.001) and behavioral health (OR 1.82, p< 0.001) having the highest odds of usage when compared to pediatrics. Having a telemedicine visit was the strongest predictor of portal usage (OR: 2.30, p< 0.001), while residence in zip codes with poor broadband internet access was associated with lower odds of portal usage (OR: 0.97, p< 0.001).
Conclusion(s):
Conclusion: While others have reported portal usage rates as high as 64% in pediatric settings, our analysis suggests proxy portal usage rates of 30% in pediatric FQHC settings, with race/ethnicity, age group, and chronic disease status being significant drivers of portal non-usage. These findings highlight the need for appropriate and responsive HIT approaches for vulnerable populations receiving care in low-resource settings.