Medical Education
Session: Medical Education 1
517 - Fostering Equity and Allyship Through Simulation (FEATS): A Novel Curriculum for Promoting Allyship in Academic Pediatric Hospital Systems
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 517
Publication Number: 517.14
Publication Number: 517.14

Joseph deBettencourt, MD (he/him/his)
Resident Physician
Ann & Robert H. Lurie Children's Hospital of Chicago
Chicago, Illinois, United States
Presenting Author(s)
Background: Discrimination, racism, and implicit bias create barriers to high-quality patient care and effective teamwork in healthcare. FEATS is an interprofessional standardized actor-based simulation curriculum designed to teach allyship skills to increase learner confidence in identifying and responding to instances of racism and bias in the healthcare setting.
Objective: Determine the impact of FEATS on participant knowledge, attitudes towards allyship, and confidence in recognizing and addressing workplace racism and bias.
Design/Methods: In this pilot study, 40 nurse educators and hospitalists at our institution agreed to participate in one of 13 FEATS sessions offered from 6/22 through 5/23. We assessed participant knowledge, attitudes, and confidence before and one month after the intervention. Response rates to the surveys were 100% (40) and 83% (33) for the pre- and post-survey. Descriptive statistics and the paired t-test (significance, p< 0.05) were used to compare pre- and post-data. We report effect size as Cohen’s d coefficient.
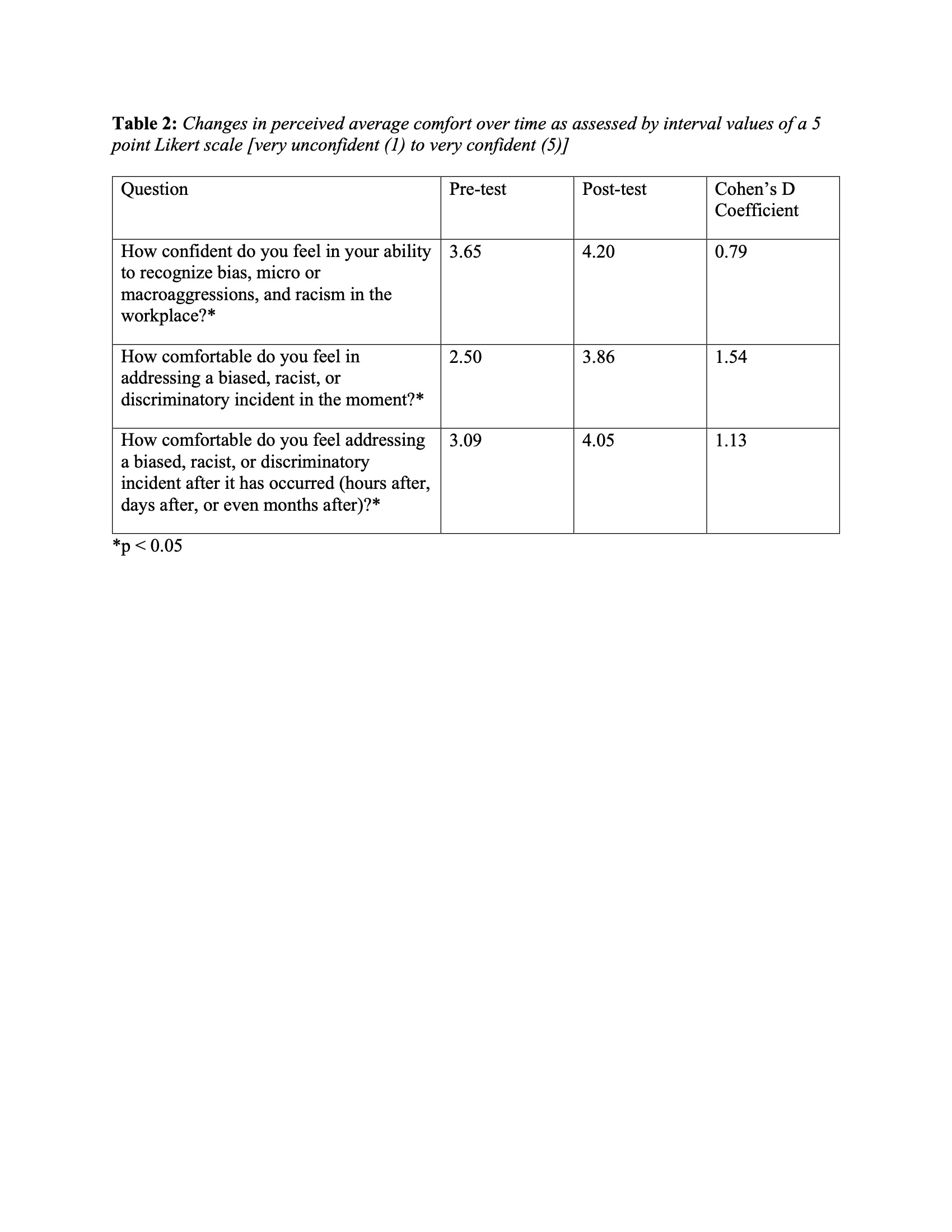
Results: Participants scored high on the knowledge section of the survey, with an average score of 94% for the pre-survey. Averaged scores increased after the intervention to 97% at one month follow-up, which was not statistically significant. Although perceived barriers to allyship remained similar before and after the intervention (Table 1), confidence in the ability to recognize biased, discriminatory, and racist behavior in the workplace and confidence in the ability to address such behaviors in the moment and after the event increased significantly with effect sizes ranging from 0.79 to 1.54 (Table 2).
Conclusion(s): This pilot study demonstrates that a novel standardized patient-based simulation is a useful tool for increasing confidence in allyship behaviors. While confidence is an imperfect proxy for future action, it is important that providers have confidence in their ability to exhibit allyship. Improved confidence may support learner action and is an area for future research. The employees who volunteered for the pilot study demonstrated considerable pre-existing knowledge surrounding terminology related to allyship, as demonstrated by the high pretest knowledge scores. Further research will be conducted on the curriculum’s impact as it is expanded to a more heterogenous group of learners. Additionally, future research is needed to determine whether our curriculum impacts hospital-wide climate.
.jpg)