Adolescent Medicine
Session: Adolescent Medicine 3
177 - Patterns and Policy Implications of Contraception Access Among Adolescents and Young Adults in the United States: Insights from the 2017-2019 National Survey of Family Growth
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 177
Publication Number: 177.21
Publication Number: 177.21

Michelle Shankar, MD (she/her/hers)
Postdoctoral Fellow
Yale University
New Haven, Connecticut, United States
Presenting Author(s)
Background: Nearly half of all pregnancies in the U.S. are unintended, and rates are highest among adolescents and young adults (AYAs). Understanding patterns in contraception access may reveal opportunities to advance reproductive health equity among AYAs.
Objective: To examine associations between sociodemographic factors and sources of contraception access among AYAs in the United States.
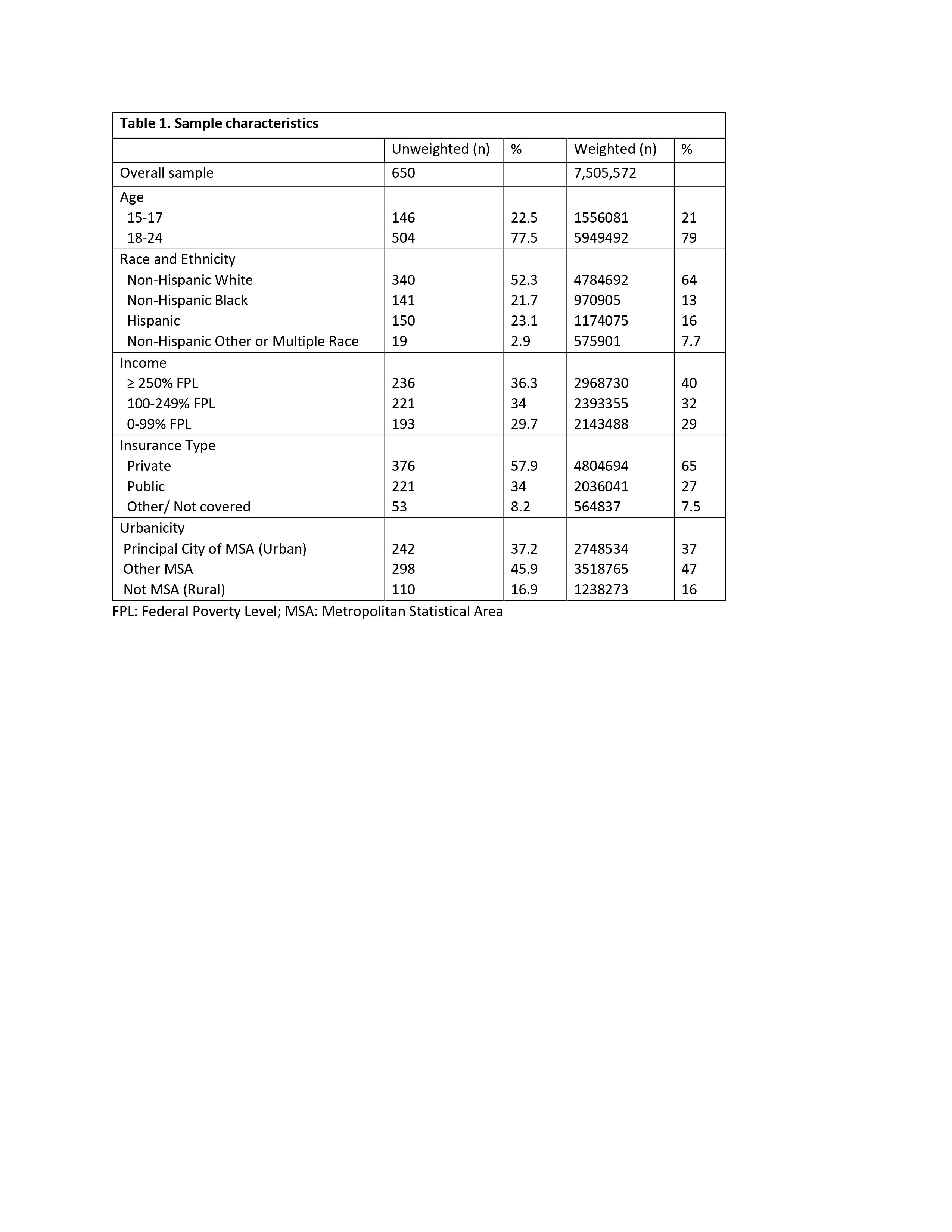
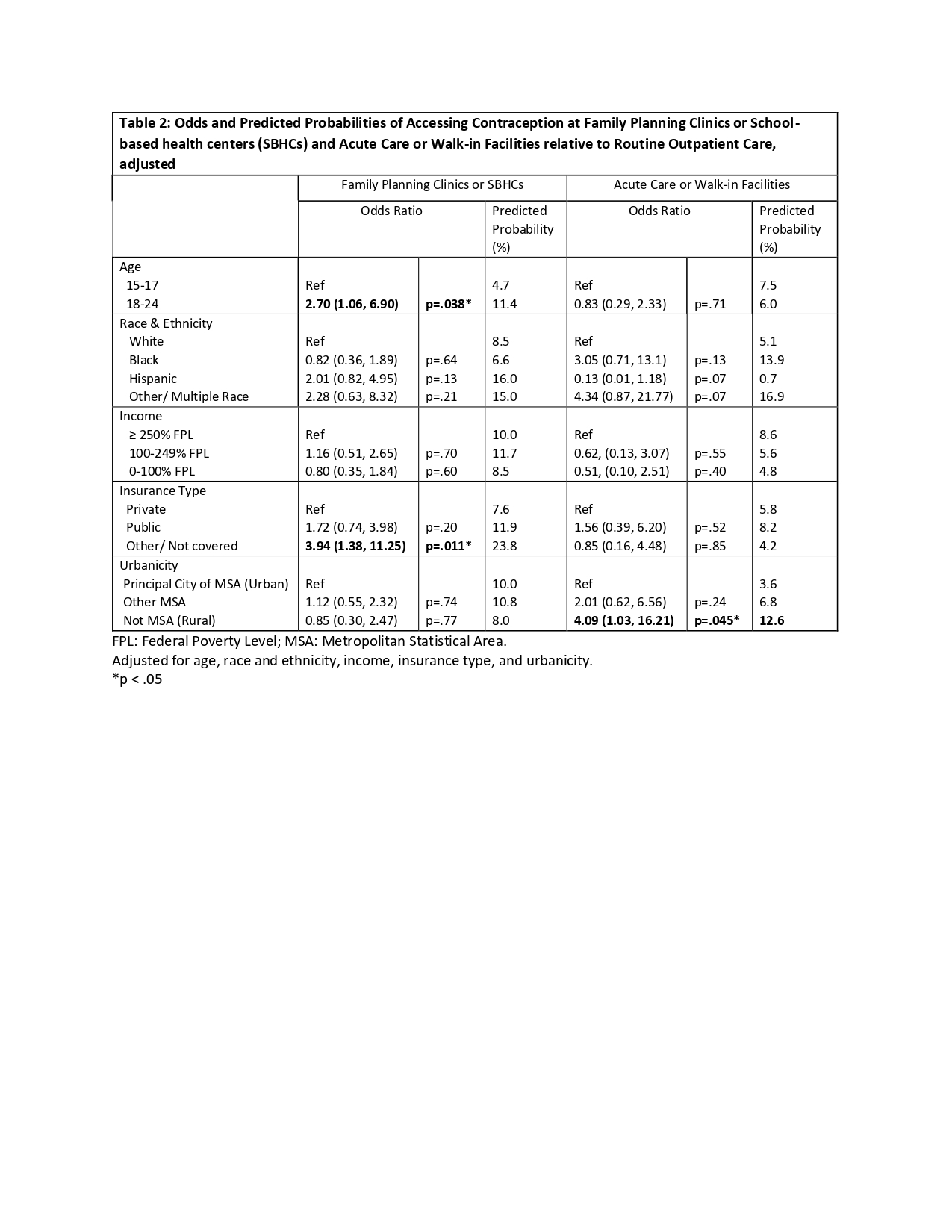
Design/Methods: In this cross-sectional study, we analyzed data from the 2017-2019 National Survey of Family Growth. Our sample included 15-24-year-old respondents who received a method of or prescription for contraception in the last 12 months (n=650). Our outcome of interest was the predicted probability of accessing contraception in routine outpatient care settings (private or public), family planning clinics or school-based health centers, and acute care or walk-in clinical settings. Exposure variables included age, race and ethnicity, household income, insurance type, and urbanicity. Using routine outpatient care settings as a reference group, we developed a multinomial regression model to identify sociodemographic factors associated with the use of family planning/SBHCs and acute care settings as sources of contraception access (odds ratios and predicted probabilities). All models were adjusted for age, race and ethnicity, household income, insurance type, and urbanicity.
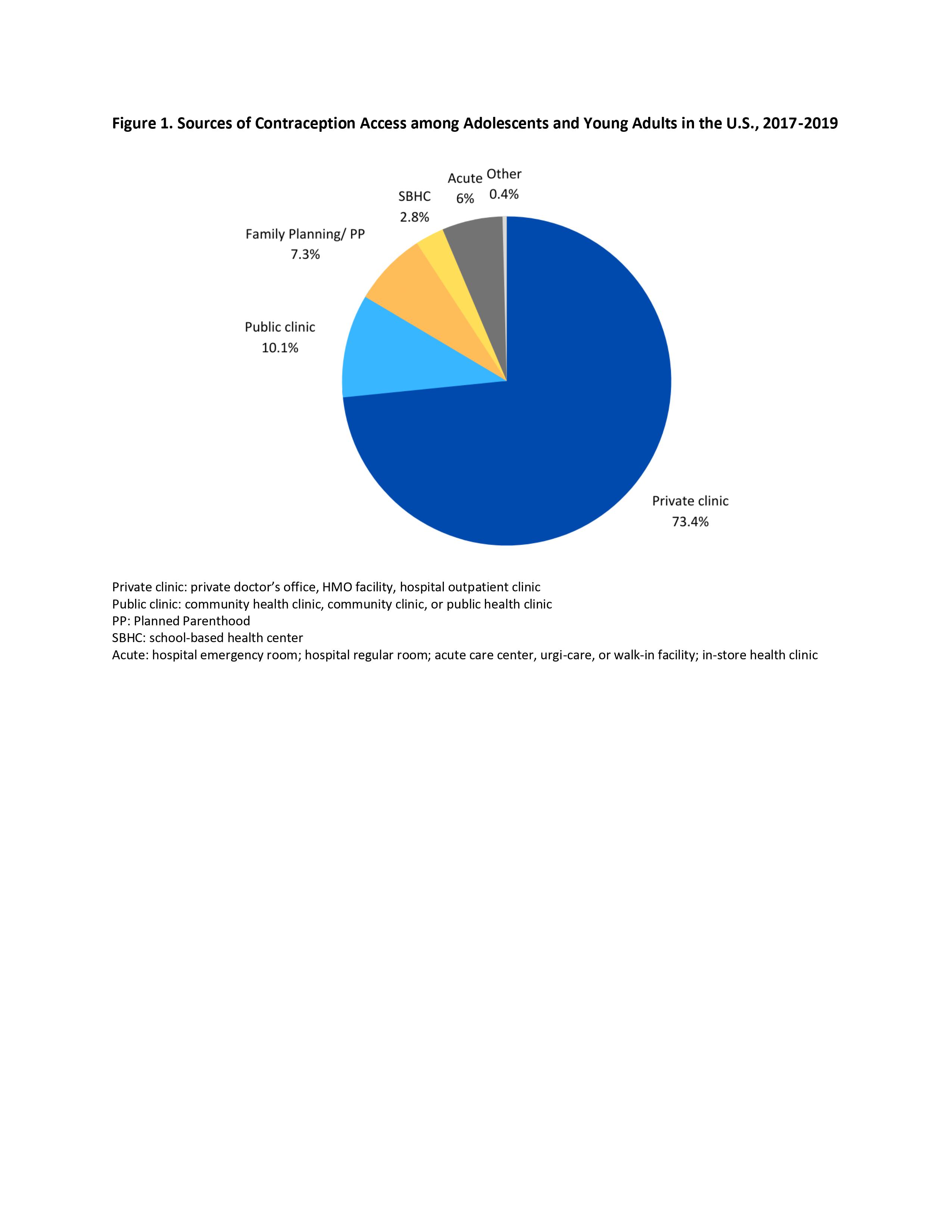
Results: The weighted survey sample represented 7,505,572 AYAs (79% 18-24 years old, 64% non-Hispanic white, 40% household income ≥ 250% federal poverty level, 65% privately insured, 37% urban, and 16% rural). Overall, 6,270,070 AYAs (83%) accessed contraception in routine outpatient care settings. After adjusting for covariates, uninsured AYAs were significantly more likely to access contraception via family planning or school-based clinics (predicted probability 23.8%) than privately insured AYA (7.6%, OR 3.94 [95% CI 1.38, 11.25]). Older AYAs were more likely (11.4%) than young AYAs (4.5%) to access contraception at a family planning or school-based clinic (OR 2.7 [95% CI 1.06, 6.89]). AYAs in rural settings were more likely (12.7%) to access contraception from acute care facilities than those in urban settings (3.6%) (OR 4.09 [95% CI 1.03, 16.21]).
Conclusion(s): The majority of AYAs accessed contraception in routine outpatient care settings, reinforcing the importance of investing in primary care for contraception delivery. Family planning and school-based health centers were important sources of care for older and uninsured AYAs. Capacity building is needed in rural areas to expand contraceptive access beyond acute care settings.