Neonatology
Session: Neonatal Infectious Diseases/Immunology 1
596 - Serum IL-6 levels predict risk of postoperative systemic inflammatory response syndrome in newborns with congenital diaphragmatic hernia
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 596
Publication Number: 596.23
Publication Number: 596.23

Takao Kobayashi, MD (he/him/his)
Clinical Fellow
Hyogo Prefectural Kobe Children's Hospital Perinatal Center
Kobe, Hyogo, Japan
Presenting Author(s)
Background: Systemic inflammatory response syndrome (SIRS) due to stress from neonatal surgery can lead to perioperative complications, including death and respiratory disorders. Interleukin-6 (IL-6) has been reported to be involved in the stress response in pediatric and adult patients. We hypothesized that serum IL-6 levels can predict risk of postoperative SIRS in newborns.
Objective: To characterize perioperative changes in serum IL-6 levels in newborns with congenital diaphragmatic hernia (CDH), and further investigate the correlation between the peak IL-6 levels and surgical stress-related factors.
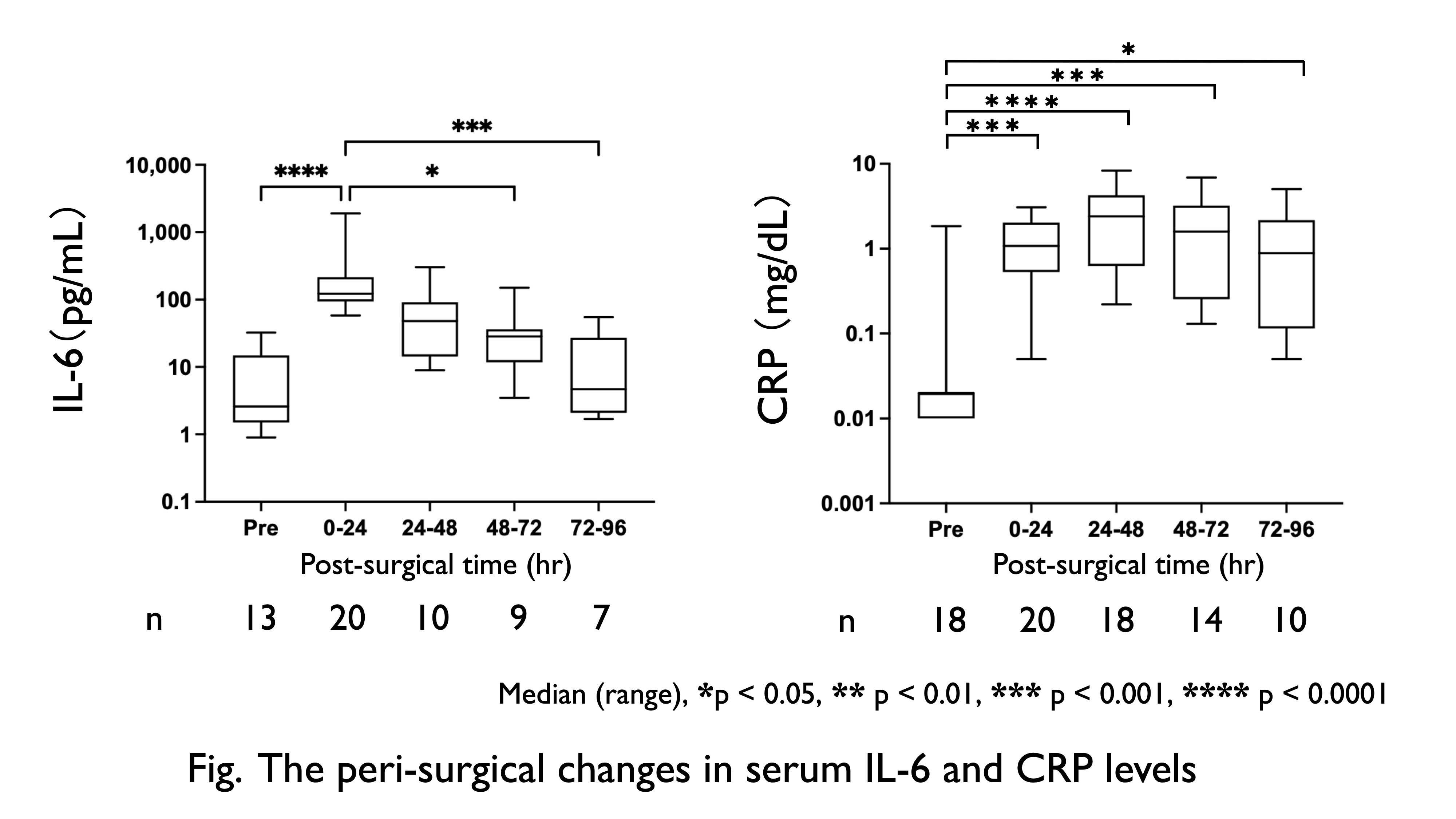
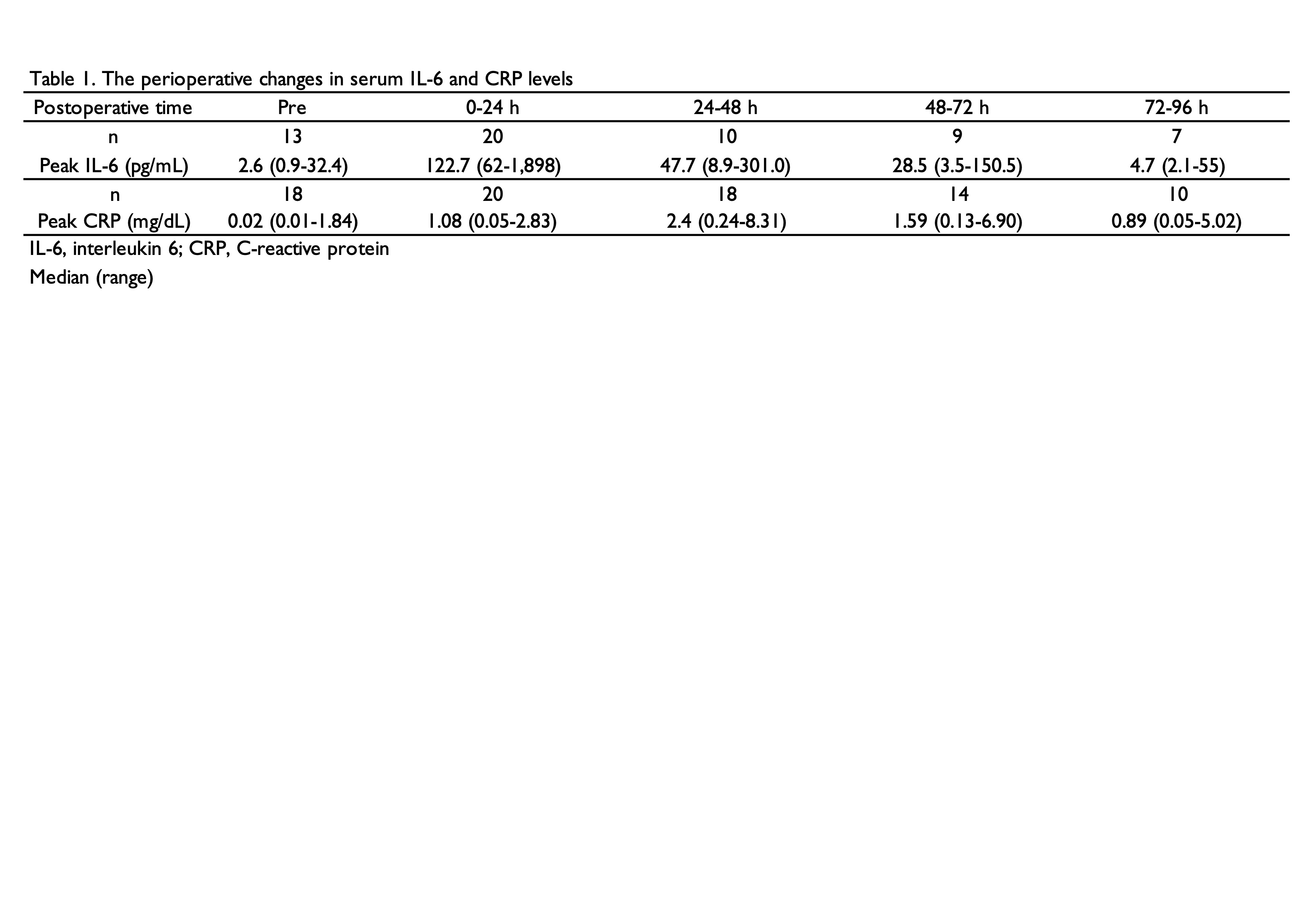
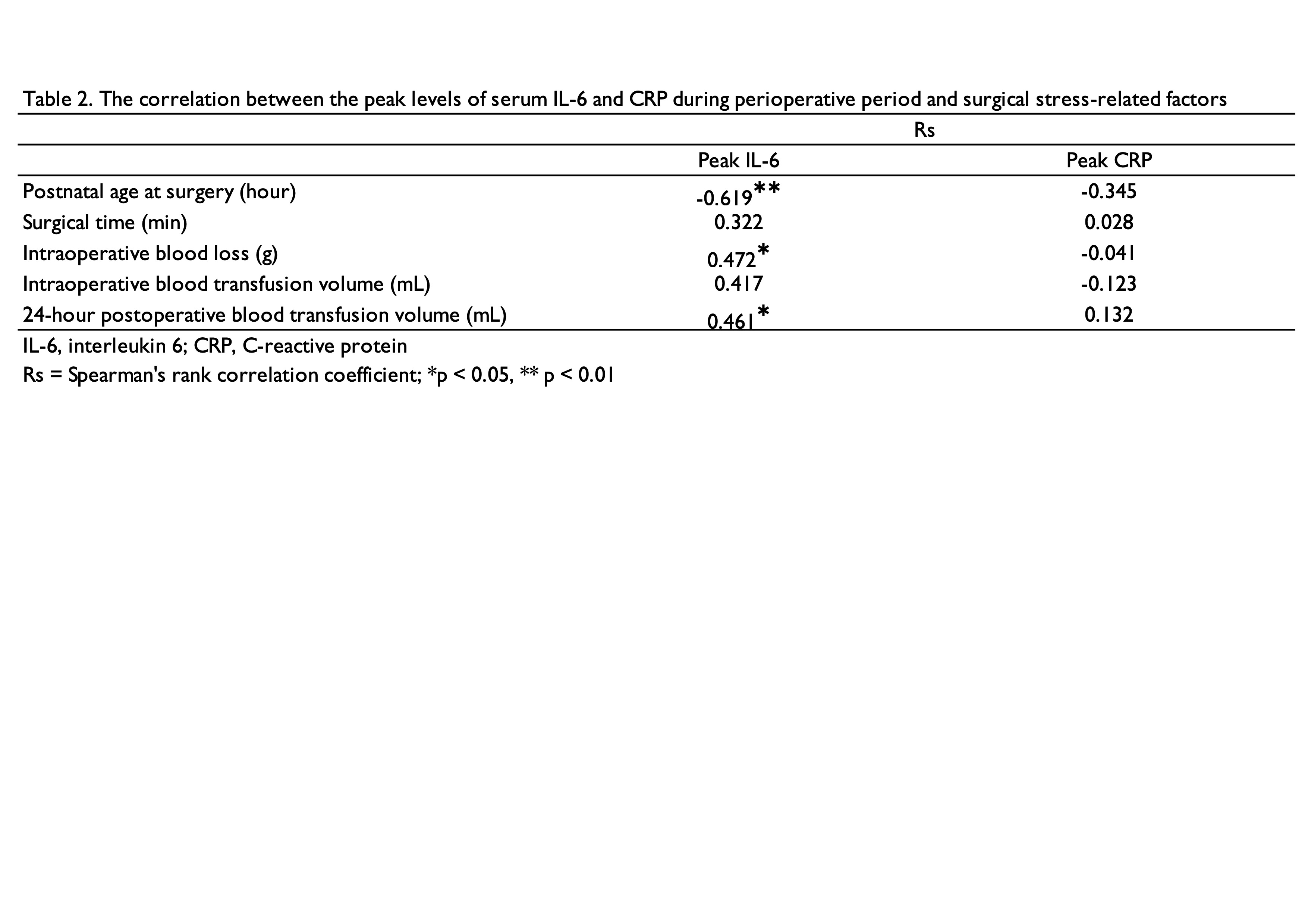
Design/Methods: n this single-center study, newborns with CDH who underwent surgical correction at our perinatal center between January 2009 and December 2022 were retrospectively studied. Serum IL-6 levels were measured using a chemiluminescent enzyme assay (Fujirebio Inc., Tokyo, Japan) or by electrochemiluminescence (Cobas e 411, Roche, Mannheim, Germany) when residual blood samples were available. Changes in serum IL-6 and C-reactive protein (CRP) levels from 72h preoperatively to 96h postoperatively were assessed. In addition, the correlation between the peak perioperative levels of serum IL-6 and CRP and surgical stress-related factors, such as postnatal age at surgery, surgical time, and volume of intraoperative blood loss (g), intraoperative blood transfusion volume (mL), and 24-h postoperative blood transfusion volume (mL) was analyzed.
Results: Among the 58 newborns with CDH, 20 cases had available data to calculate changes in serum IL-6 and CRP levels. We found that serum IL-6 levels peaked [median: 122.7 (62-1,898) pg/mL] at 10h (1-42) postoperatively; while CRP levels [median: 2.40 (0.24-8.31) mg/dL] peaked at 38h (12-47) postoperatively (Table 1). Peak serum IL-6 levels had a significant negative correlation with postnatal time (rs = -0.619) and a significant positive correlation with volumes of intraoperative blood loss and 24-h postoperative transfusion (rs = 0.486 and 0.516, respectively). Peak serum CRP levels had no significant correlations with any surgical stress-related factors (Table 2).
Conclusion(s): In newborns with CDH, serum IL-6 levels peak early postoperatively, and correlate with surgical stress-related factors. Despite being retrospective study with small sample size, we speculate that serum IL-6 levels may predict risk for postoperative SIRS.