Neonatology
Session: Neonatal Quality Improvement 5
83 - Initiating Bubble CPAP in the Delivery Room: A Component of a Quality Improvement Initiative to Decrease Chronic Lung Disease
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 83
Publication Number: 83.3322
Publication Number: 83.3322

Sara Stucker, MD (she/her/hers)
Neonatal-Perinatal Medicine Fellow
University of Minnesota
Minneapolis, Minnesota, United States
Presenting Author(s)
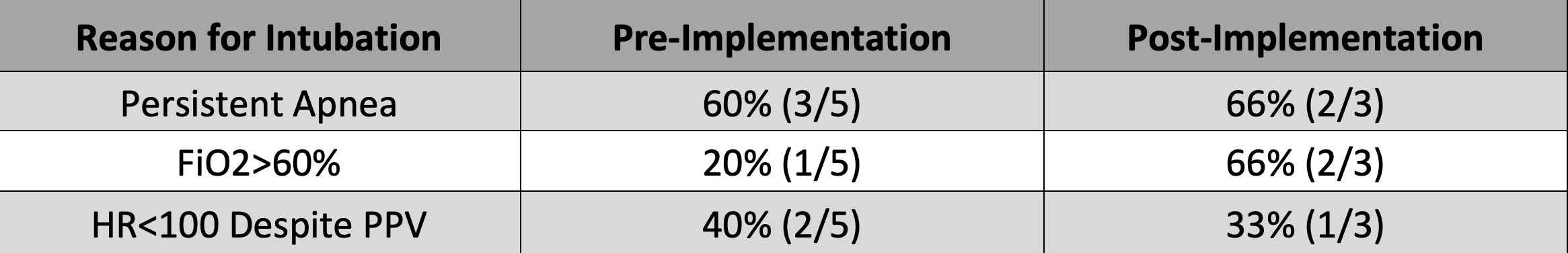
Background: Although multifactorial, intubation and mechanical ventilation are associated with chronic lung disease (CLD). To encourage avoidance of intubation, current guidelines at our level IV regional perinatal center state that infants ≥ 26w0d should be stabilized on continuous positive airway pressure (CPAP) in the delivery room (DR) and only intubated for prolonged apnea, persistent FiO2 > 60% or heart rate < 100 despite positive pressure ventilation (PPV). Despite these guidelines, our center has high rates of intubation, with 91% of infants less than 30 weeks’ gestation intubated during their hospitalization according to Vermont Oxford Network (VON) data. Prior to project implementation, a T-piece resuscitator and face mask were used for PPV and CPAP in the DR until infants were transitioned to bubble CPAP (BCPAP) upon admission to the neonatal intensive care unit (NICU).
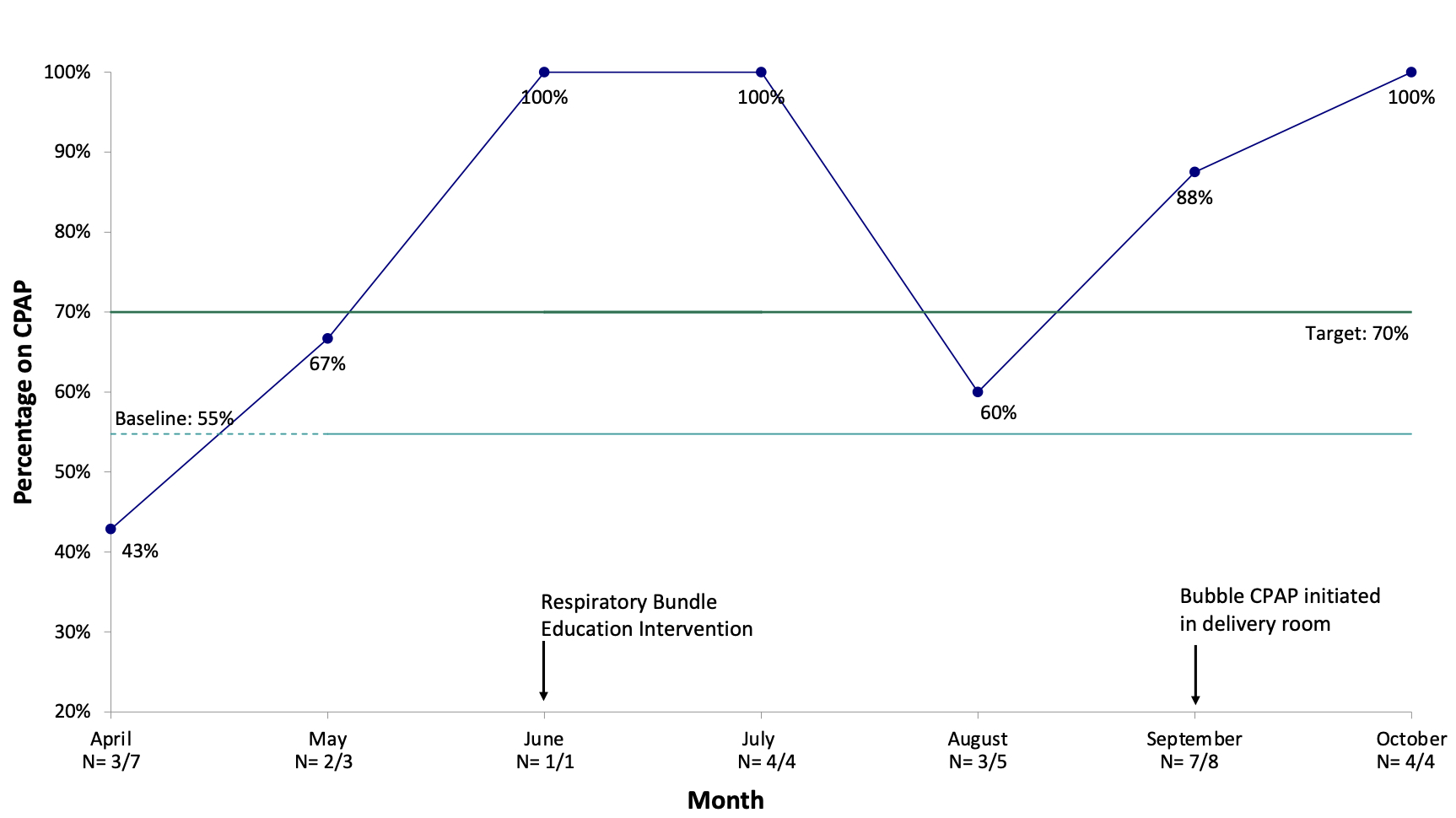
Objective: To increase the percentage of infants 26-29 weeks’ gestation leaving the DR on CPAP from 55% to 70% by December 2023.
Design/Methods: A multi-disciplinary team including physicians, advanced practice providers, nurses, respiratory therapists and unit leadership developed interventions for this quality improvement (QI) initiative to decrease CLD.
Phases: Baseline DR information was collected from 3/2023-5/2023. Staff education occurred 6/2023- 8/2023 and initiation of BCPAP in the DR began 9/2023.
Interventions:
1) Staff education to increase compliance to current DR CPAP guidelines.
2) Initiate BCPAP in the DR rather than upon admission to the NICU.
Measures: Process measures include rate of delivery room survey completion, rate of infants 26-29 weeks’ gestation leaving the DR on CPAP, and indication if intubation occurred. Outcome measures include DR intubation rate.
Results: The percentage of infants 26-29 weeks’ gestation leaving the DR on CPAP increased from a baseline of 55% to a monthly average of 90% in the 5 months post project initiation (Figure 1). DR surveys were completed for 86% (66/77) of infants. Reported reasons for intubation are presented in Table 1.
Conclusion(s): Implementation of a QI initiative to promote early stabilization of premature infants with CPAP has increased our unit’s compliance with the standard of care and reduced rates of early intubation in the delivery room.