Hospital Medicine
Session: Hospital Medicine 2
317 - Clinical chaRacteristics and outcomEs of hospitAlized children with Acute resPiratory infecTions: the READAPT-Kids study cohort
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 317
Publication Number: 317.24
Publication Number: 317.24

Peter J. Gill, MD, DPhil, MSc (he/him/his)
Staff Physician, Scientist
The Hospital For Sick Children
Toronto, Ontario, Canada
Presenting Author(s)
Background: After the relaxation of SARS-CoV-2 related public health interventions, there was a surge of hospital admissions in children with respiratory tract infections. Little is known about the epidemiology of these cases, including the causative viral pathogens, severity of illness, and complications.
Objective: To describe sociodemographic characteristics, clinical presentation, etiology, management, and clinical outcomes of children under the age of 18 years admitted to tertiary care pediatric hospitals with acute respiratory infections.
Design/Methods: Observational cohort of children (0-18 years) hospitalized with acute respiratory infections at two large Canadian children’s hospitals from July 1, 2022 to December 31, 2022. Cases were identified using ICD-10-CA codes before manual screening for inclusion by trained research assistants. Detailed clinical and demographic information were extracted, including clinical outcomes and complications such as length of hospital admission, pediatric intensive care unit (PICU) admission, need for invasive mechanical ventilation, disposition, and death.
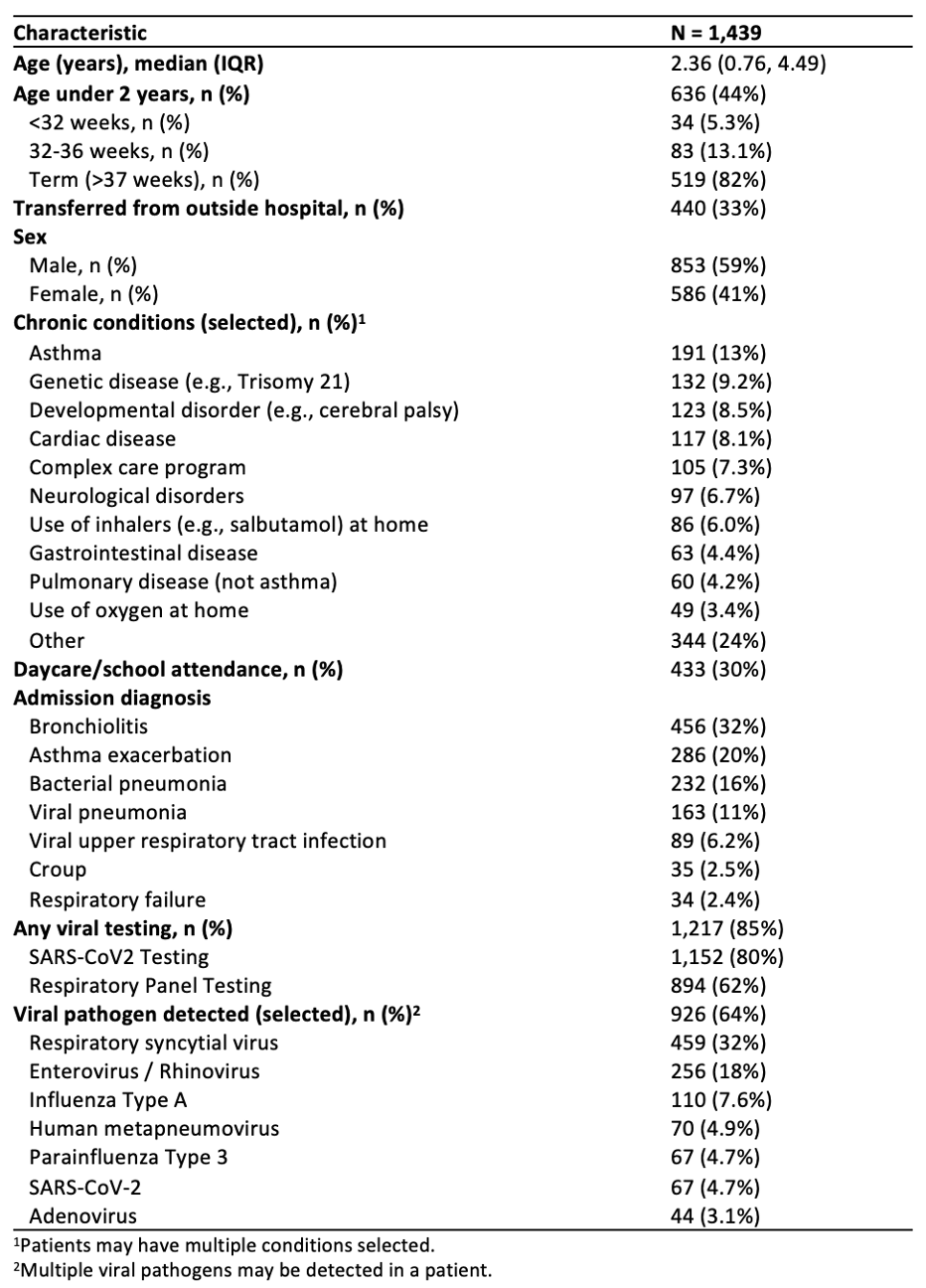
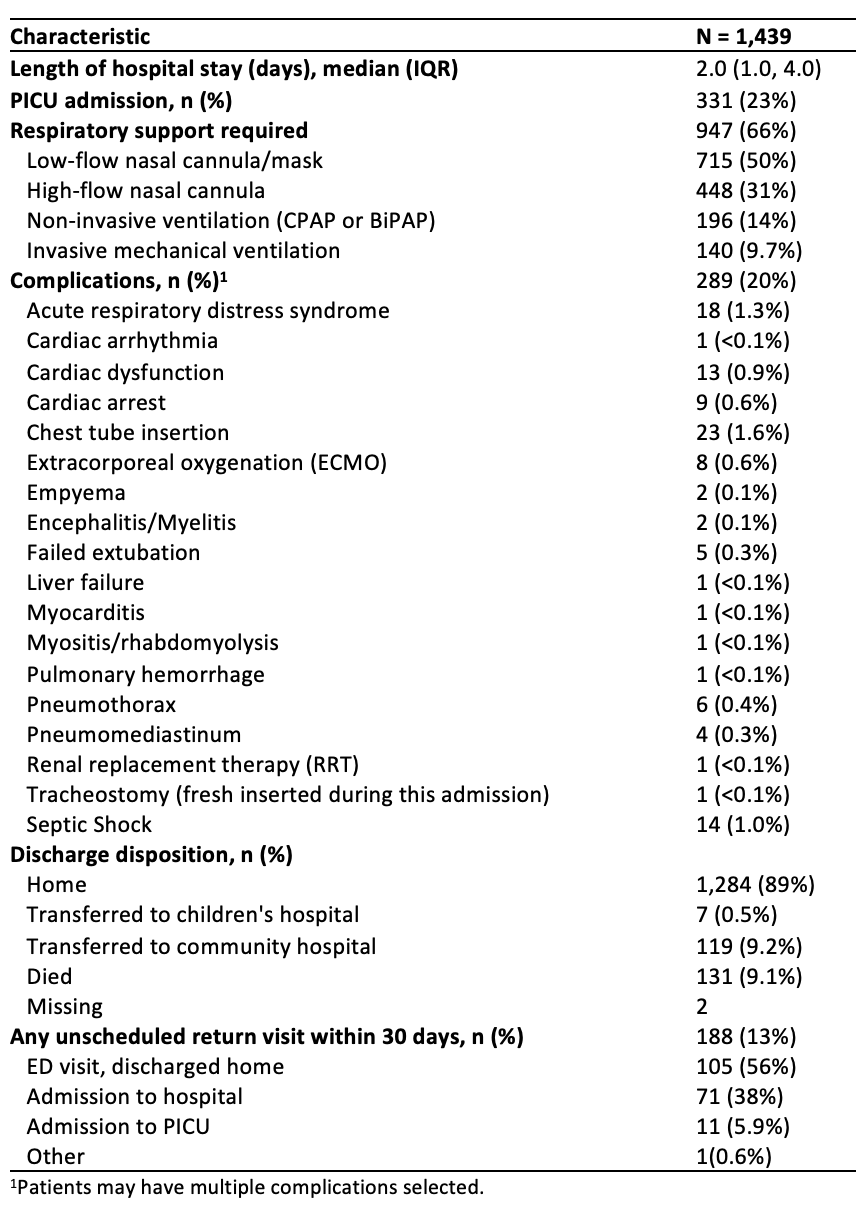
Results: There were 1439 hospital admissions, of which 853 were male (59%) and a median age of 2.4 years (IQR 0.8-4.6 years) (Table 1). Asthma was the most common chronic health condition reported (13%, n=191). The most common admission diagnoses included bronchiolitis (32%), asthma exacerbation (20%), bacterial pneumonia (16%) and viral pneumonia (11%). One third (33%, n=440) of patients were transferred from an outside hospital. The most common viral pathogen identified was Respiratory Syncytial Virus (RSV) (32%, n=459), followed by Enterovirus / Rhinovirus (18%, n=256); 194 patients (13%) tested positive for two viruses, and 35 (2.4%) for three viruses. Median length of stay was 2 days (IQR 1-4 days), and 23% (n=331) were admitted to the PICU (Table 2). Two thirds (66%, n=947) of patients required respiratory support, including low flow oxygen (50%), high flow nasal cannula (33%), non-invasive ventilation (14%) and invasive ventilation (9.7%). 15 patients died. Unscheduled revisits within 30 days occurred in 188 patients (13%), including 90 re-admissions to hospital.
Conclusion(s): After the relaxation of public health interventions, most hospital admissions were in young children under the age of 5 years with bronchiolitis, asthma, and pneumonia. RSV and Enterovirus / Rhinovirus were detected in half the admissions. While most admissions were short, nearly one-quarter of children were admitted to PICU and 10% required invasive ventilation.