Technology
Session: Technology 1
175 - The effect of an Automated Patient Engagement Solutions (APES) on step-by-step parental communication around time of discharge and length of stay
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 175
Publication Number: 175.1704
Publication Number: 175.1704
- SH
Susan Henderson, MA, CPXP (she/her/hers)
Director of NICU Parent Support
Indiana University School of Medicine
Indianapolis, Indiana, United States
Presenting Author(s)
Background: Digital patient engagement platforms are being recognized as an innovative and efficient way to increase patient engagement and optimize healthcare outcomes. Application of automated patient engagement solutions (APES) have not been previously studied in the neonatal intensive care unit (NICU).
Objective: To determine the effects of a newly implemented step-by-step automated messaging pathway on parental communication around time of discharge to home and length of hospital stay (LOS), and to compare the outcomes of infants admitted in the year preceding the intervention with the ones admitted in the year following APES at discharge (APES-D) implementation.
Design/Methods: This quasi-experimental study took place in a level 4 NICU at Riley Hospital for Children, Indianapolis, Indiana. The APES-D used Twistle by Health Catalyst as the secure automated messaging platform to send timed messages, educational documents, and videos to parents of infants preparing for discharge to home. The “Baseline” group included eligible infants admitted in the year prior APES-D implementation on January 18, 2022. “Intervention” group included infants admitted in the year following tool implementation. “Intervention” group was further divided into the post-intervention “APES-D Nonuser” group (comprising infants of parents who opted out APES -D), and the “APES-D User” group (comprising infants of parents who used the APES-D).
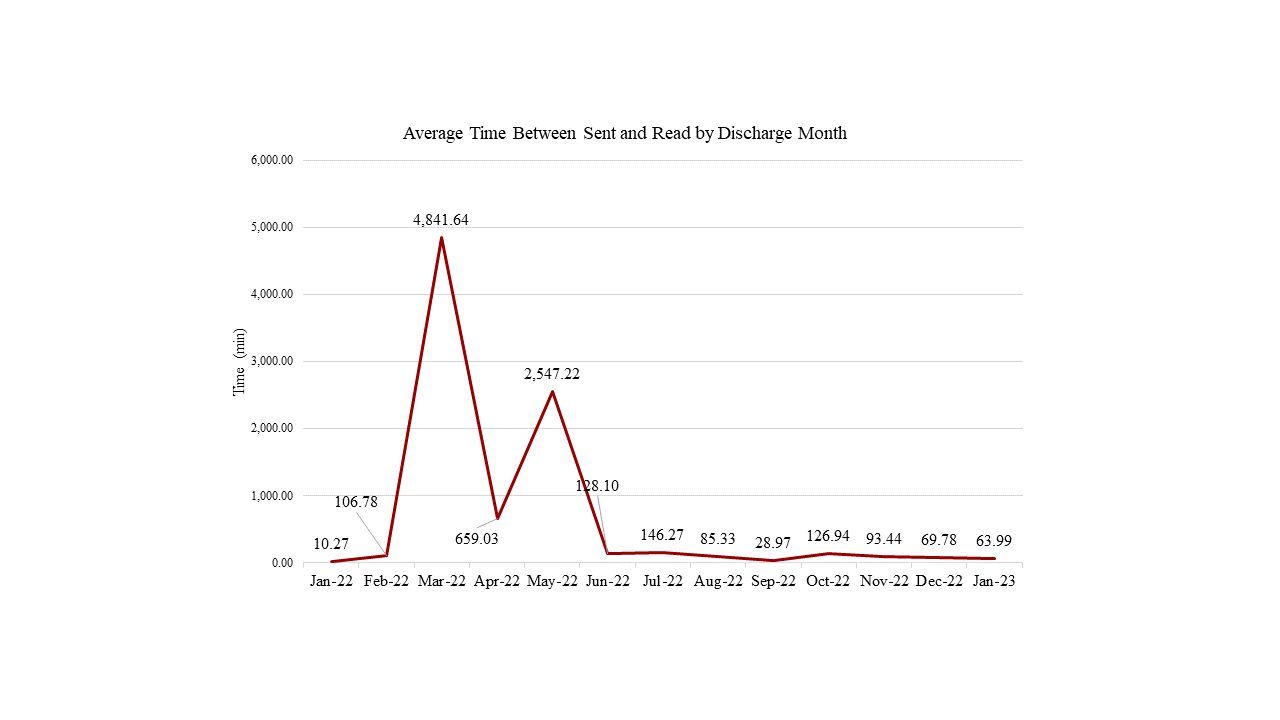
Results: Baseline infant characteristics in the APES-D User versus Nonuser study groups were similar except birthweight and primary language (Table 1). LOS was significantly shorter in APES-D User compared to APES-D Nonuser group (median 15.08 vs 22.72, p=0.003; Table 2). Length of stay was significantly longer in infants covered by public or combined public/private insurance than in those with private only or self-pay (Table 2). The average time between the APES-D message-received and message-read during the intervention period is shown in Figure 1. “Baseline” and “Intervention” study groups were similar with regard to LOS and patient socio-demographics with the exception of primary language (p=0.013).
Conclusion(s): Ours is the first quasi-experimental cohort study that aimed to understand critical engagement sociodemographic factors in APES utilization in the NICU. APES-D was associated with shorter NICU LOS however the tool utilization was strongly influenced by social determinants of health. Future research is needed to identify all contextual factors and mechanisms that are associated with effective APES utilization to optimize discharge to home without socioeconomic disparity.
.png)
.png)
