Neonatology
Session: Neonatal Follow-up 3
540 - Medications for Gastroesophageal Reflux in Extremely Preterm Infants and Associations with Growth and Development
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 540
Publication Number: 540.3318
Publication Number: 540.3318
.jpg)
Chelsea O. Lockyear, MD (she/her/hers)
Neonatal-Perinatal Medicine Fellow
Duke University School of Medicine
Durham, North Carolina, United States
Presenting Author(s)
Background: Use of acid-suppressive therapy for gastroesophageal reflux treatment in the neonatal intensive care unit (NICU) has changed in recent years because of safety concerns. We sought to evaluate the association of acid-suppressive therapy with growth and development in a contemporary cohort of preterm infants.
Objective: Determine associations of acid-suppressive therapy with growth and development in extremely preterm infants.
Design/Methods: Cohort study of infants < 27 weeks gestational age born at Neonatal Research Network centers between July 1, 2012 and December 31, 2019 who survived to discharge. Infants with major congenital anomalies or missing follow up at 22-26 months corrected age were excluded. Infants were divided into 2 groups: those discharged home on acid-suppressive therapy (defined as proton pump inhibitors and/or histamine-2 receptor antagonists) and those who were not. Demographics, clinical features, and outcomes between groups were compared. Outcomes of interest included z-scores for weight, length, and head circumference (HC), and moderate-severe neurodevelopmental impairment (NDI) at 22-26 month follow up. To estimate the association of acid-suppressive therapy with these outcomes, linear mixed models and generalized linear mixed models were used to control for predefined characteristics as fixed effects, with sites as random effects.
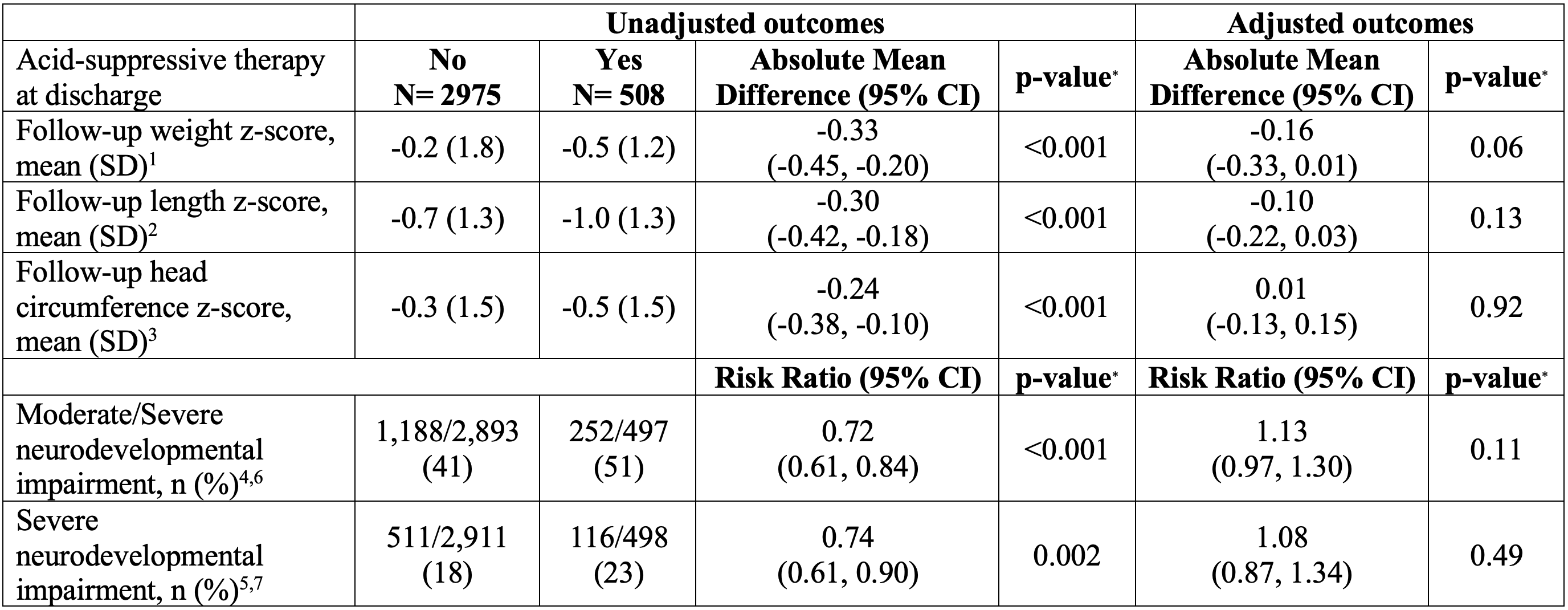
Results: Of 3,483 infants that met inclusion criteria, 508 (15%) were discharged on acid-suppressive therapy (Table 1). Acid-suppressive therapy at discharge was more frequent among infants who were small for gestational age or had necrotizing enterocolitis, bronchopulmonary dysplasia, gastrostomy tube dependence, or a Nissen procedure (Table 1). Use at discharge decreased from 18% in 2012 to 11% in 2019 (Figure 1, p=0.01). At follow up, 9% of infants were on acid-suppressive therapy, 66% of whom were not discharged on it (Table 1). When adjusted for pre-determined covariates, no difference was found in growth or moderate-severe NDI at follow up between the two groups (Table 2). The absolute mean difference in adjusted weight z-score was -0.16 (p=0.06, Table 2), and relative risk of moderate to severe NDI was 1.13 (p=0.11, Table 2).
Conclusion(s): Following adjustment for potential confounding, we observed no association between acid-suppressive therapy and growth or neurodevelopment. From 2012-2019, fewer infants were discharged on acid-suppression, and were more likely to have had a complex hospital course. Clinical trials of post-discharge acid-suppressive therapy are needed.
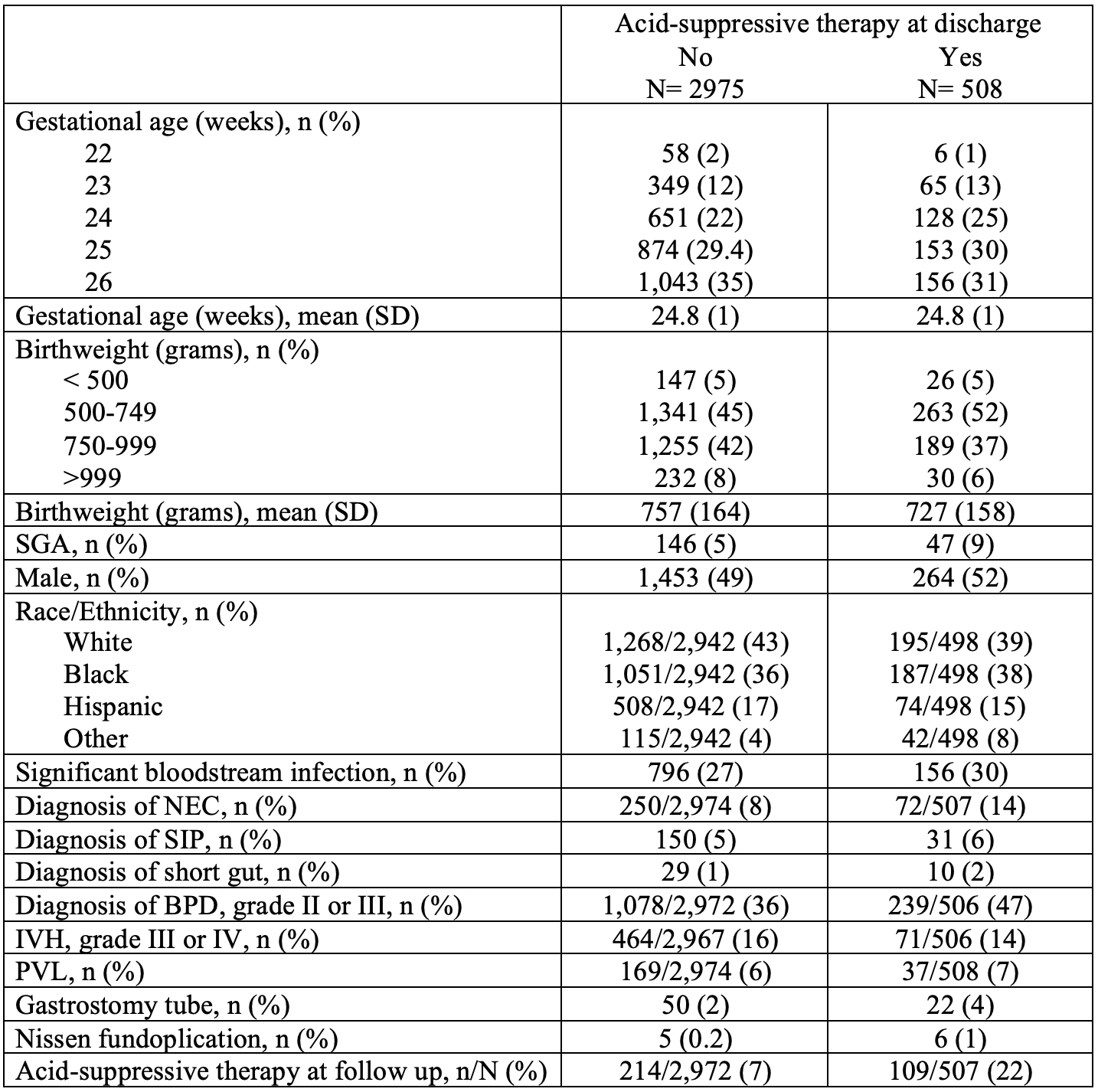
Figure1.jpeg