Hospital Medicine
Session: Hospital Medicine 2
319 - Evaluating Nursing Perspectives To Promote Surgical Co-Management In Pediatrics
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 319
Publication Number: 319.38
Publication Number: 319.38

Rachita Gupta, MD (she/her/hers)
Pediatric Hospital Medicine Fellow
Children's Hospital Colorado
Aurora, Colorado, United States
Presenting Author(s)
Background: Surgical co-management (SCM), a model in which hospitalists and surgeons share responsibility in caring for surgical patients, has been implemented at some pediatric institutions to optimize perioperative care for medically complex patients. SCM has led to improved communication amongst providers and reduced complications, medical errors, and length of stay. SCM began at our institution in 2004 for complex spine patients and has since expanded to other patient subgroups. Nursing staff (RNs) play a crucial role in communicating with different providers to consolidate care for SCM patients. Data are lacking in the literature on RN views of pediatric SCM.
Objective: To evaluate RN perspectives on SCM at a free-standing children’s hospital.
Design/Methods: With the aid of a survey methodologist, a 16 question survey was designed to assess RN preferences and comfort with SCM. Since SCM patients are admitted to the medical-surgical floor of our institution, this REDCap survey was issued via an email link to all RNs who worked on that floor in November 2021. The survey remained open for 40 days with three follow-up reminder emails sent to non-responding RNs. Data were analyzed descriptively using frequencies and percentiles.
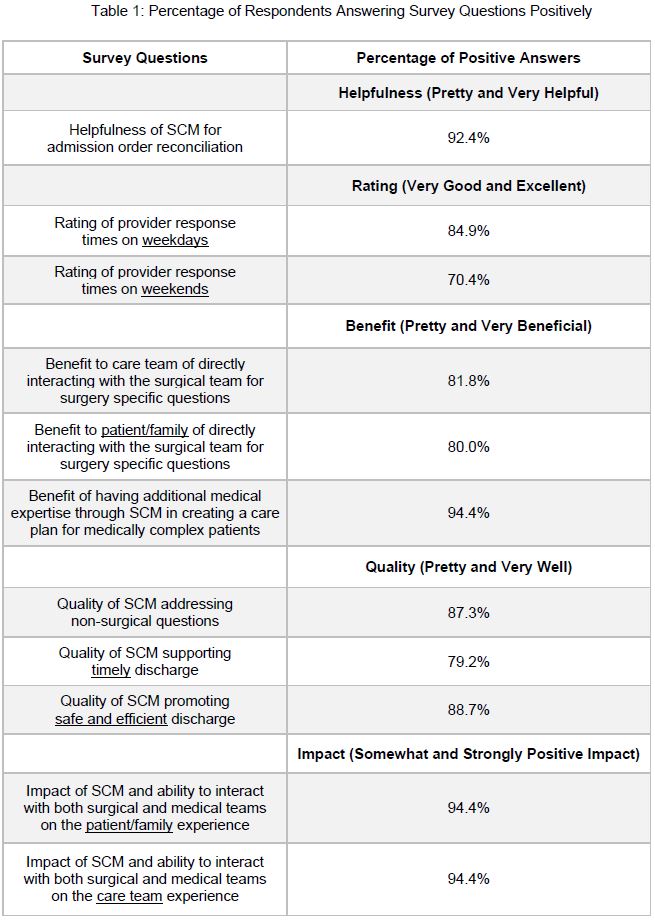
Results: Sixty of 134 RNs responded to the survey (44.8%). Most respondents (92%) had managed at least one SCM patient and were eligible to complete the rest of the survey. 94.4% of RNs said SCM was “pretty” or “very” beneficial for having additional medical expertise in creating a care plan (Table 1). 92.4% felt that SCM was “pretty” or “very” helpful for admission order reconciliation. 94.4% of RNs reported a “somewhat” or “strongly” positive impact of SCM on the patient/family experience and on the care team. 79.2% and 88.7% of RNs reported that SCM supports timely and safe/efficient discharge “pretty” or “very” well respectively. Open ended comments revealed that RNs felt more content with the faster response times, providers’ overnight availability, and improved communication with patients and team members.
Conclusion(s): Overall, RNs reported high satisfaction levels and benefits to patient safety, communication with the care team, timeliness, care effectiveness, and patient/family experience with pediatric SCM. This study supported the development of a formal SCM inpatient team, thus separating SCM patients from non-surgical patients on other inpatient teams, to optimize perioperative care for medically complex patients. Further research is needed to assess whether pediatric SCM benefits patient outcomes such as clinical deterioration events, pain management, and readmission rates.