Palliative Care
Session: Palliative Care
160 - Analyzing EMR Documentation of Goals of Care Conversations Occurring in the Neonatal Intensive Care Unit
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 160
Publication Number: 160.1655
Publication Number: 160.1655
- EB
Emil Bielecki, MD (he/him/his)
Neonatal-Perinatal Medicine Fellow
Rush Medical College of Rush University Medical Center
Chicago, Illinois, United States
Presenting Author(s)
Background: Goals-of-care conversations (GOCC) in the neonatal intensive care unit (NICU) are associated with reduced family anxiety levels and improve delivery of care aligning with parental preference. Extremely premature infants have higher rates of comorbidities such as necrotizing enterocolitis (NEC), severe bronchopulmonary dysplasia (BPD), and grade 3-4 intraventricular hemorrhage (IVH). How often these conversations occur in the NICU and whether their prevalence differs by patient diagnosis and sociodemographic factors is unknown.
Objective: (1) To determine how often GOCC occur during the NICU hospitalization for a high-risk neonatal cohort and how often goals/values, prognostic information, and end-of-life preferences are documented in the electronic medical record (EMR). (2) Assess impact of sociodemographic and medical factors on documentation of GOCC in the NICU.
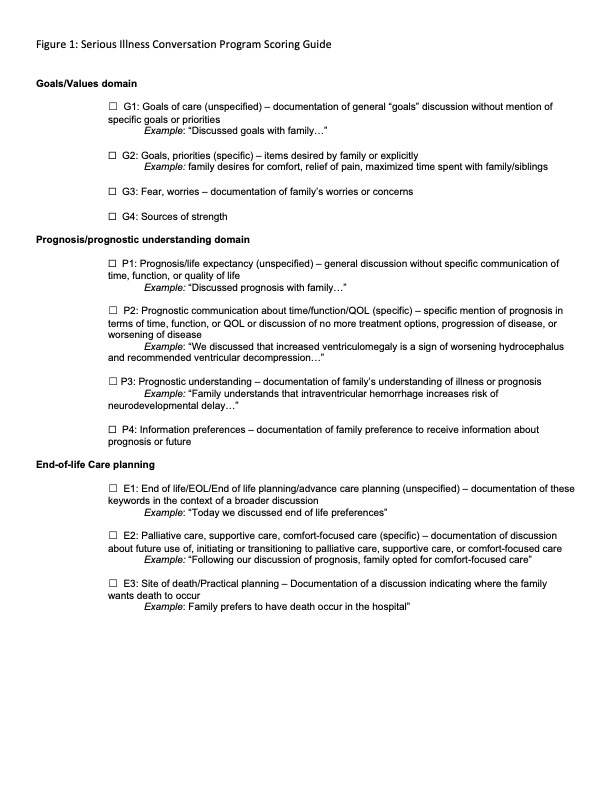
Design/Methods: This is a retrospective review of NICU GOCC at an academic tertiary care center from January 1, 2018 through December 31, 2021. To select a high-risk neonatal cohort who would benefit from GOCC, inclusion criteria included birth gestational age ≤ 27 weeks or birth weight (BW) ≤ 1000 g. GOCC were determined by manual review of EMR notes with quality of conversation scored using the Serious Illness Conversation Program Modified Codebook (see Figure 1). Patients were grouped based on presence of at least one meeting note and continuous and categorical medical and sociodemographic factors were compared. We compared prevalence and predictors of GOCC using multivariable logistic regression adjusted for sociodemographic factors.
Results: 174 patients met inclusion criteria, of whom 38% (66/174) had at least one meeting documented in the EMR . Patients receiving meetings were more premature, lower BW, and had higher incidence of severe BPD and grade 3-4 IVH (see Table 1). Independent of other variables, patient factors associated with meeting occurrence include male sex, low BW, and presence of severe BPD and grade 3-4 IVH. Multivariable generalized mixed models failed to show that sociodemographic and medical factors impact total documentation score.
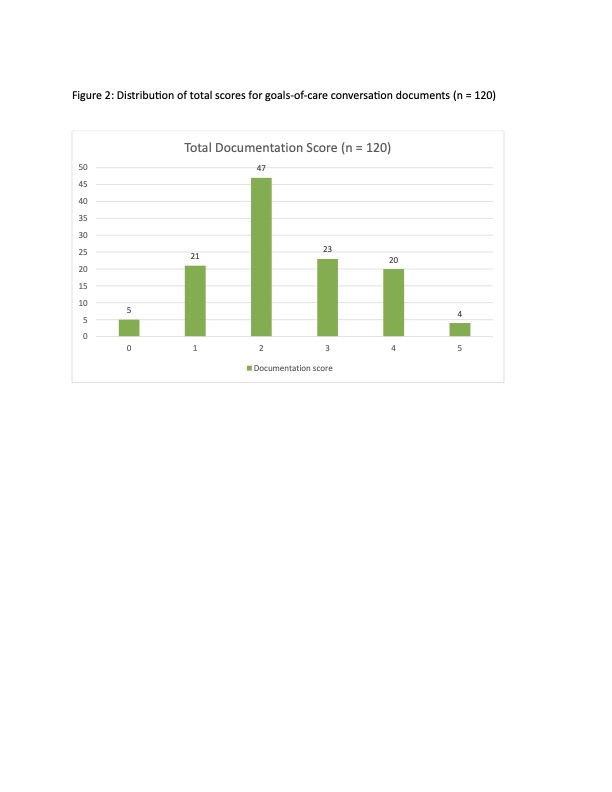
Conclusion(s): A minority of patients had at least one meeting documented and their documented content varied significantly as scores ranged from 0 to 5 points with a mean score of 2.37 points (see Figure 2). Patients receiving meetings were more premature and sicker; however specific comorbidities were not associated with a higher score. Additional study is needed to determine whether exploration of family goals of care improves neonatal care outcomes and levels of family distress.
.jpg)