Neonatology
Session: Neonatal Infectious Diseases/Immunology 2
612 - Systemic Antifungal Utilization among Extremely Low Birth Weight Infants from 2009-2021
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 612
Publication Number: 612.57
Publication Number: 612.57
Dustin D. Flannery, DO, MSCE
Assistant Professor of Pediatrics
Children's Hospital of Philadelphia
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: AAP Redbook recommends fluconazole prophylaxis for extremely low birth weight infants (ELBW, < 1000g BW) in NICUs with high rates of invasive fungal infections (IFI), as opposed to universal prophylaxis, due to lack of survival benefit in trials. There is debate, however, about criteria for antifungal prophylaxis, and contemporary antifungal prescription data among ELBWs is lacking.
Objective: To assess antifungal use across a large cohort of ELBW infants admitted to academic and community NICUs across the US over 13-years and compare infants with and without early fluconazole prophylaxis
Design/Methods: Retrospective cohort study of inborn ELBW infants admitted to a NICU in the Premier Database from 2009-2021. Annual proportions of infants receiving at least one dose of systemic fluconazole, amphotericin, and/or echinocandin, were determined and average annual absolute changes were estimated using generalized linear regression. Demographics and clinical characteristics were compared between infants with and without early fluconazole prophylaxis, defined as ≥2 doses in the 7 days after birth, and risk of mortality between groups was determined using logistic regression.
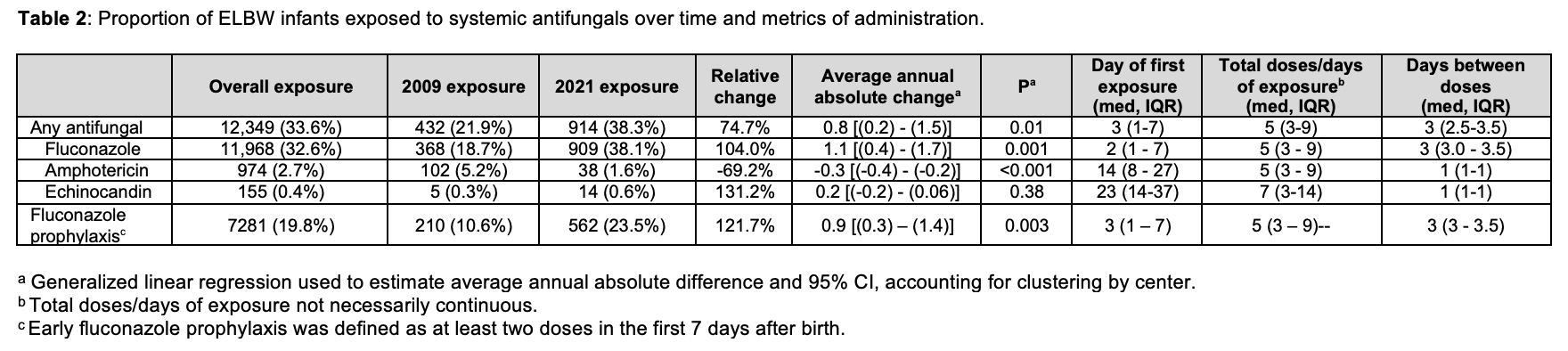
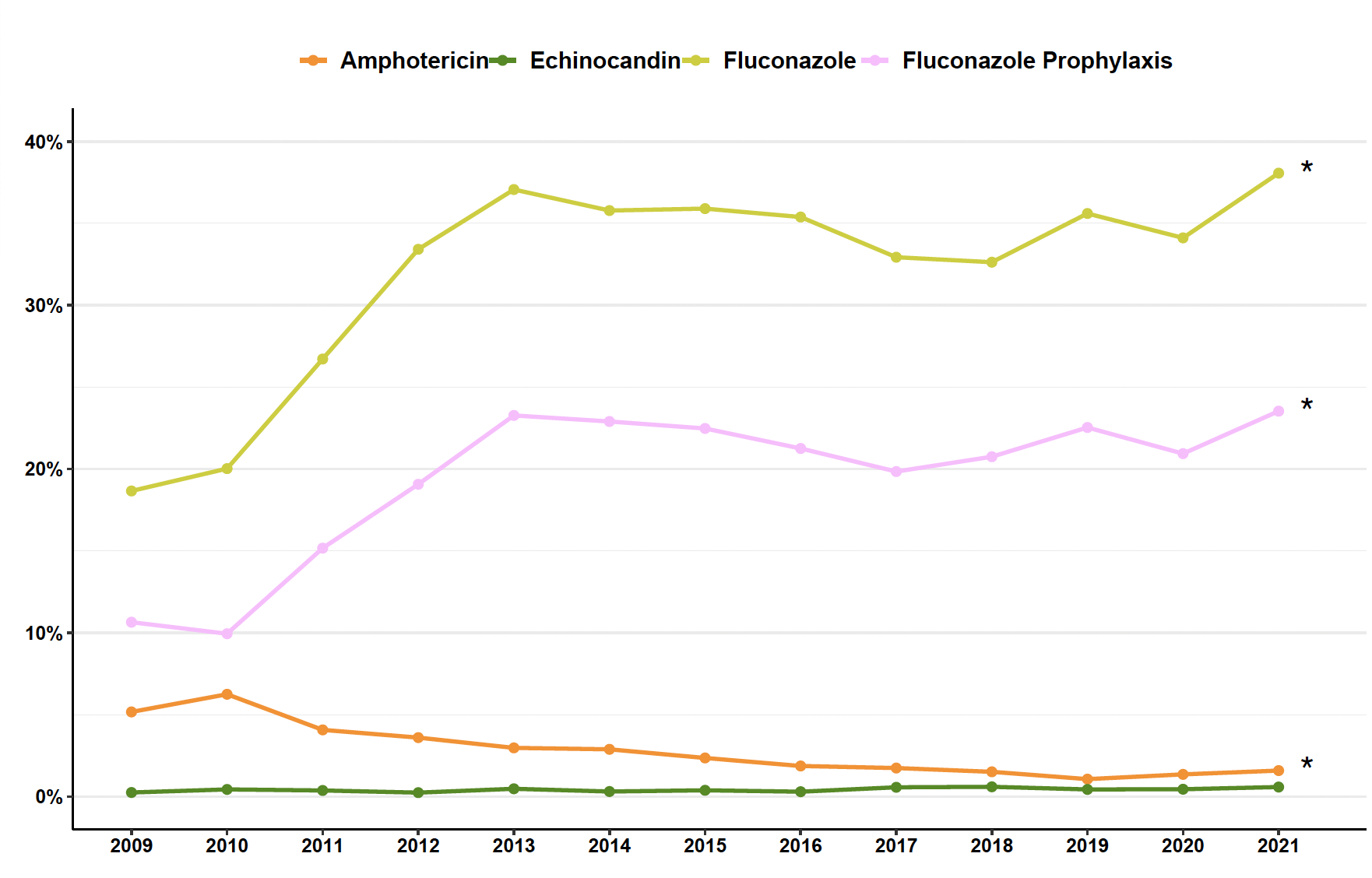
Results: From 2009-2021, 36,701 ELBW infants were admitted to 402 NICUs (Table 1); 34% received an antifungal at any time, with an increase from 22% in 2009 to 38% in 2021 (p < 0.01). Fluconazole use increased by 104% and amphotericin use decreased by 69%, both with statistically significant annual trends (Table 2 and Figure). Echinocandin use was low (0.4%) and did not change over time. Median first day of exposure, days between doses, and total doses are shown in Table 2. ELBW infants who did not receive early fluconazole prophylaxis (80%), compared to those who did (20%), had higher GA, shorter length of stay, and lower rates of later antifungal treatment (Table 1). After adjusting for sex, race, ethnicity, and GA, ELBW infants without prophylaxis had increased risk of death before discharge (aRR 1.8 [95% CI 1.7,1.9]; p< 0.001).
Conclusion(s): Among this large ELBW cohort, fluconazole use nearly doubled and amphotericin use decreased by more than two-thirds from 2009-2021. Usage patterns suggest fluconazole is used primarily as prophylaxis, while amphotericin and echinocandins are used as empiric and/or therapeutic treatment for IFI. Infants without early fluconazole prophylaxis had higher adjusted risk of mortality, contradictory to earlier trials. Further studies including microbiology data are needed to understand the impact of early antifungal prophylaxis on patient-level outcomes.
.png)