Medical Education
Session: Medical Education 9
512 - Transfer Validity Testing of a VR UVC Simulation
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 512
Publication Number: 512.3302
Publication Number: 512.3302
- TG
Taylor Gohman, DO (he/him/his)
Neonatal Fellow
University of Illinois College of Medicine at Peoria
Peoria, Illinois, United States
Presenting Author(s)
Background: Residents have fewer opportunities to practice neonatal procedures due to duty hour restrictions, ACGME’s requirement of only 2 neonatal intensive care block rotations and variable exposure to procedures on actual patients. Procedural opportunities require time, expert oversight, possible danger to patients and potential requirement of simulation laboratories that are not all consistently available at Residency Programs. A simulation solution
for Residents’ lack of procedural skill experiences must be developed to meet this need.
Objective: To establish the transfer validity of a virtual reality (VR) emergent umbilical venous catheter simulation (UVC).
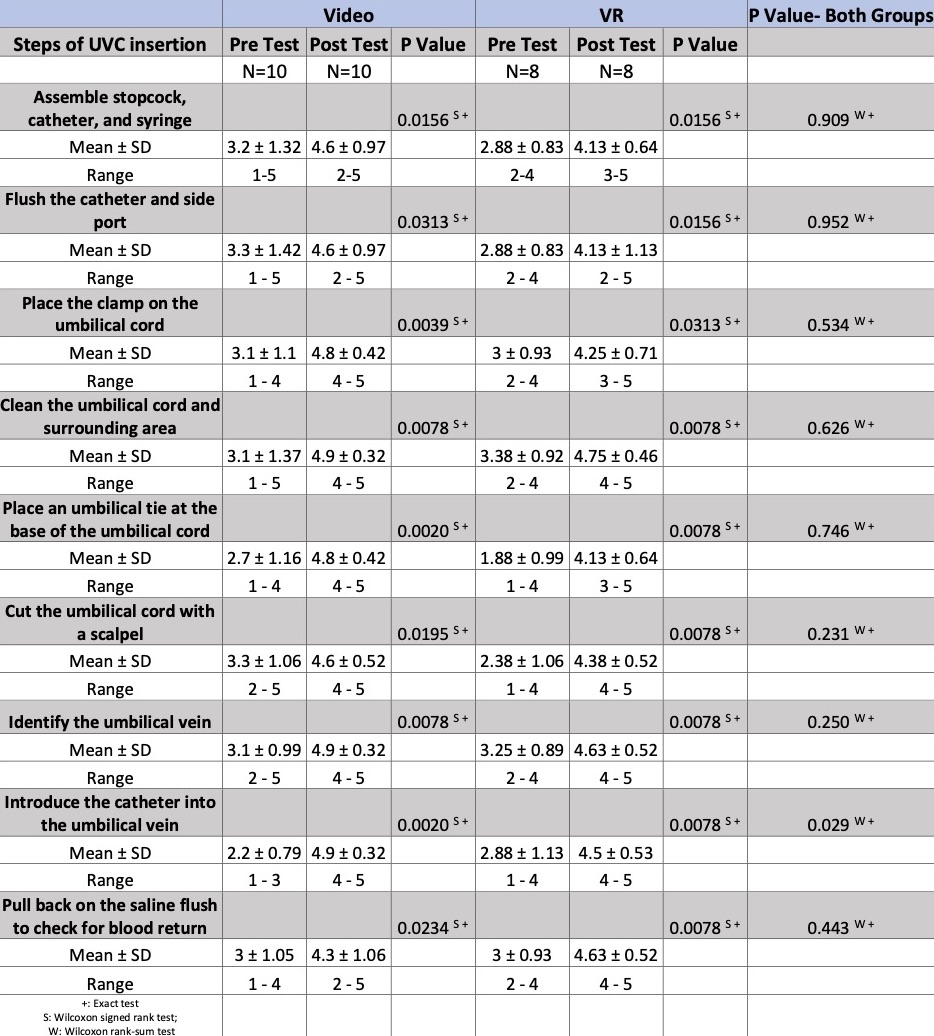
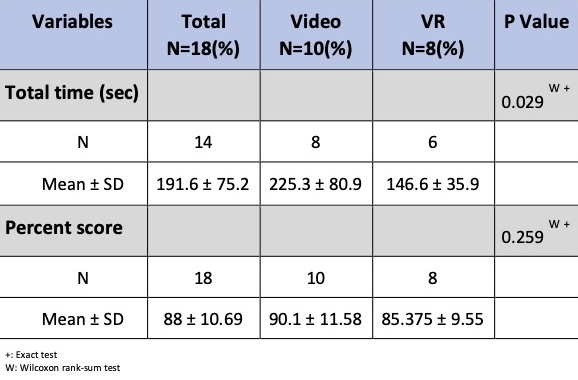
Design/Methods: Eighteen Pediatric and Medicine/Pediatric Residents were randomized to either watch a video of UVC placement or use a VR simulation module. Every Resident completed a pre-evaluation of their comfort in performing each step of UVC placement. Immediately after completing their respective educational intervention, Residents were scored and timed while placing a UVC on a manikin. Every Resident then completed a post-evaluation of their comfort in performing the UVC procedure. Room for comments was available for the VR group.
Results: Both the video and VR groups had improved comfort in performing the steps of UVC insertion after completing their educational intervention. There was no difference between the video and VR groups in the degree of improvement from pre/post evaluation. The VR group performed the UVC procedure on the manikin slightly faster than the video group (p= 0.029).There was no difference in the total score between the video and VR groups, both scoring over 85% correct.
Conclusion(s): Both video and VR groups experienced improved comfort in performing the steps of UVC placement after educational intervention. Residents in both groups performed well when inserting a UVC into a manikin, thus demonstrating the transfer validity of the VR UVC simulation. Even though the VR group’s speed was statistically significant when performing the UVC procedure on the manikin, this may not be clinically significant. Repeat assessment of participants after 5-9 months is currently underway. Future work will be needed to determine if there are differences in long-term retention of skills between the video and VR groups.