Neonatology
Session: Neonatal Quality Improvement 4
68 - Reduction in Benzodiazepine Usage in Patients Born Less than 25-weeks' Gestation
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 68
Publication Number: 68.3293
Publication Number: 68.3293

Matthew H. Merves, MD
Associate Professor
University of Arkansas for Medical Sciences/Arkansas Children's Hospital
Little Rock, Arkansas, United States
Presenting Author(s)
Background: The provision of intensive care for newborns as early as 22 weeks of gestation has become commonplace. Opioids and benzodiazepines (BZ) are widely used in the neonatal ICU to provide analgosedation in those mechanically ventilated. While the preterm infant brain is susceptible to adverse effects of pain and stress, studies have also demonstrated that exposure to BZ can harm the developing brain.
Objective: To reduce cumulative BZ exposure in babies born less than 25-weeks' gestation.
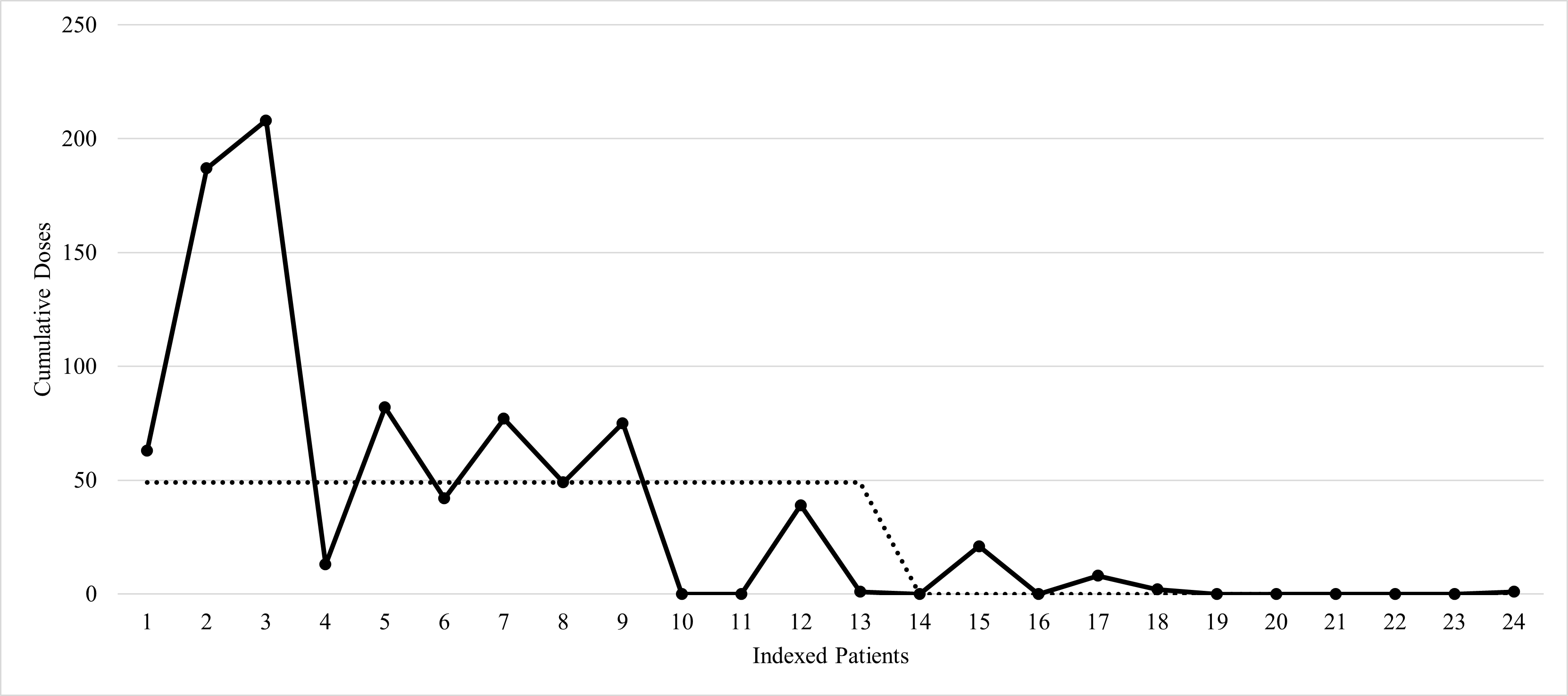
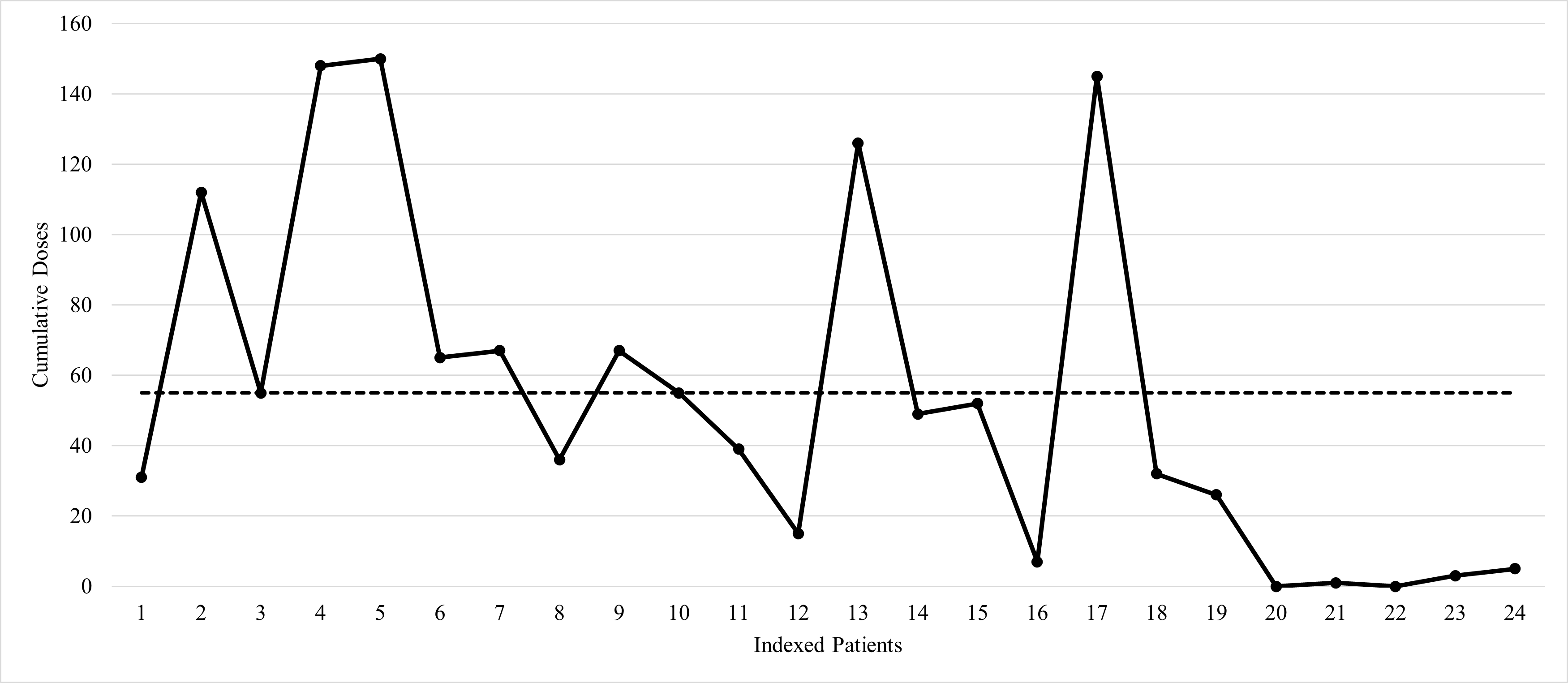
Design/Methods: We conducted a multi-intervention quality improvement (QI) initiative to reduce BZ exposure among babies born less than 25-weeks' gestation at our level III delivery hospital (DH), and in the case of our level IV referral center (RC), admitted within 24 hours of birth. The outcome measure of cumulative number of BZ doses within the first 90 days of life, the balancing measure of opiate exposure, and key metrics such as timing of the first dose of BZ, were all tracked in a novel, IRB-exempt tiny baby database (TBD). TBD tracks various demographics, medications, and morbidities of these patients less than 25-weeks' gestation. Baseline retrospective data obtained prior to interventions, which included creation of local care guidelines, order sets, and nursing education, as well as ongoing prospective data were collected and analyzed in the form of indexed patients who survived at least 90 days. Median values are reported with descriptive statistics used.
Results: Baseline data were collected for DH (n=13) and RC (n=19) to measure the number of BZ doses administered during the first 90 days of life, timing of the first administered dose, and the morphine milligram equivalents (MME) during this period. Post-intervention data for the DH (n=11) and RC (n=5) were compared to their respective baseline to assess the impact of implemented process changes. A Mann-Whitney U Test determined that the observed reduction of BZ doses in the first 90 days of life were statistically significant for both DH [U(Npre = 13, Npost = 5), z = 3.01, p< 0.05] and RC [U(Npre = 19, Npost = 5),z = 3.38, p< 0.001]. There was an observed increase in the balancing measure, opiate exposure, at both sites with statistical significance at DH.
Conclusion(s): A multicenter QI approach utilizing targeted interventions demonstrated reduction in BZ exposure. The observed increase in opiate exposure could indicate a potential shift in practice that warrants further review. Development of a TBD establishes a foundation for data collection and systematic improvements in care for one of medicine’s most vulnerable populations.
.png)