Neonatology
Session: Neonatal Quality Improvement 5
80 - Improving Completion of Red Reflex Examinations at Discharge from the Neonatal Intensive Care Unit: A Practice Improvement Initiative
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 80
Publication Number: 80.3295
Publication Number: 80.3295

Grant J. Shafer, MD (he/him/his)
Physician
CHOC Children's Hospital of Orange County
Fullerton, California, United States
Presenting Author(s)
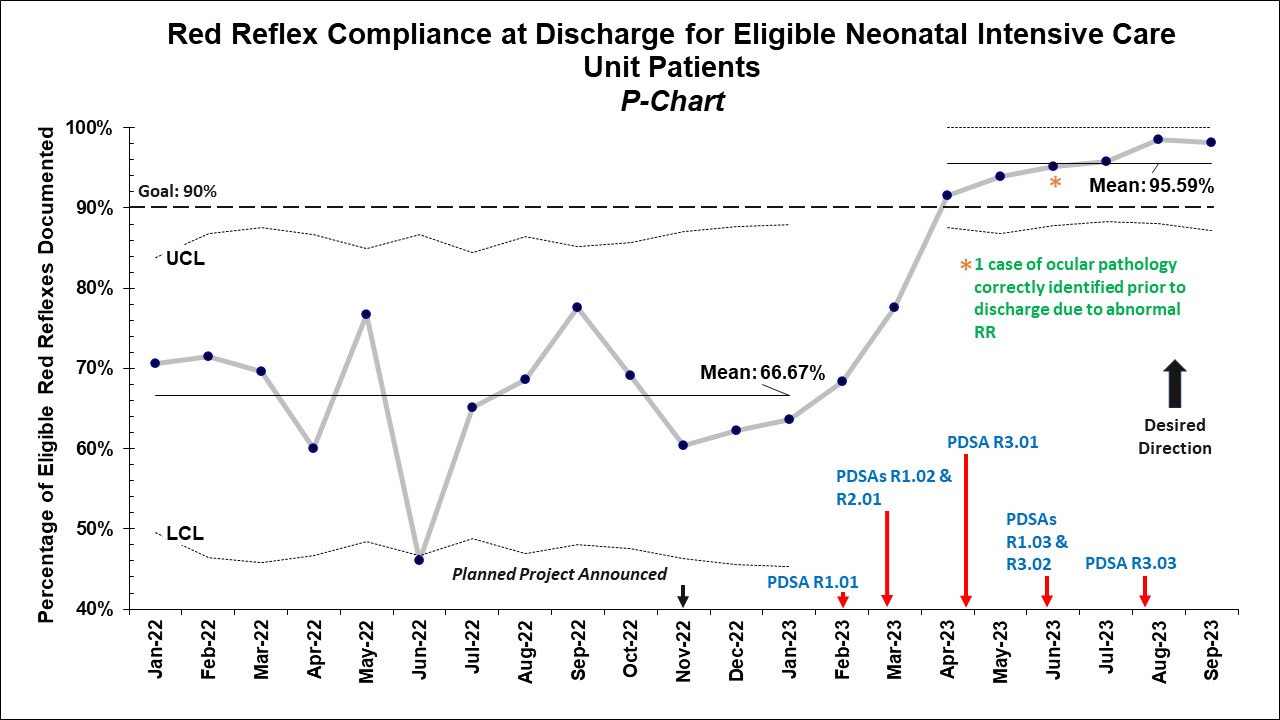
Background: Evaluation for a red reflex (RR) in the eyes of a newborn is a critical diagnostic component of the neonatal exam. Failure to perform this screen can lead to diagnostic errors with delayed identification of ocular abnormalities with the potential for visual impairment. The American Academy of Pediatrics recommends a RR exam be performed on all newborns prior to discharge. Many patients in the neonatal intensive care unit (NICU) undergo a formal ophthalmologic exam during their stay (either for retinopathy of prematurity or other indication) – which negates the need for a RR exam. However, all patients who do not receive a formal eye evaluation should have a RR exam prior to discharge. A review of all NICU discharges for thirteen months at our institution demonstrated that only 66% of eligible patients had a RR documented at any time prior to discharge with two delayed diagnoses of ocular pathology. This prompted us to initiate a practice improvement initiative to improve this rate.
Objective: To improve completion of a RR exam by discharge for eligible patients in the NICU at CHOC Children’s from baseline 66% to >90% by December 2023.
Design/Methods: We created a key-driver diagram and summarized possible interventions to achieve our aim. We have implemented various interventions over multiple plan-do-study-act (PDSA) cycles targeted towards education of NICU clinicians and trainees, electronic health record reminders, and development of a formalized workflow (including discharge checklist and optimized ophthalmoscope availability) to ensure completion of a RR exam prior to discharge. A factorial design/planned experimentation phase is anticipated to start soon which will include two additional sites – a Level IV NICU at another children’s hospital and a Level III NICU at a community affiliate hospital.
Results: After completion of seven PDSA cycles, the rate of RR completion improved from the baseline 66% to sustained >95%. Since the initiation of this initiative, one case of ocular pathology has been appropriately identified prior to discharge due to an abnormal RR exam.
Conclusion(s): Implementation of this initiative has led to an improvement in RR examination rates as well as prompt identification of ocular pathology in one case at our institution. Data collection and a multi-site factorial design/planned experimentation remain ongoing, and we anticipate presentation of additional results at the 2024 PAS Conference.