Emergency Medicine
Session: Emergency Medicine 10: Trauma
399 - Improving emergency department trauma care through an interdisciplinary, low-fidelity simulation program
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 399
Publication Number: 399.3288
Publication Number: 399.3288

lea Dikranian, MD (she/her/hers)
Pediatric Emergency Medicine Fellow
Children's Hospital of Michigan
Royal Oak, Michigan, United States
Presenting Author(s)
Background: Unintentional injuries continue to pose a significant risk to pediatric patients, emphasizing the critical need for effective trauma care and comprehensive resuscitation strategies involving the mastery of non-technical skills (NOTECHS). However, current practice often overlooks crucial NOTECHS, resulting in a deficit in teamwork, communication, and process efficiency. To address this gap, we focused on improving 5 key NOTECHS categories (leadership, cooperation, communication, assessment/decision-making, and situational awareness) recognizing the role of simulation-based training in fostering these skills.
Objective: Our study aimed to enhance the quality of trauma care in the emergency department (ED) by integrating trauma simulation cases. Additionally, we sought to evaluate and improve closed-loop communication through the validated Trauma-NOTECHS (T-NOTECHS) tool.
Design/Methods: Conducted over 9 months at a level 1 pediatric hospital, our prospective study involved bi-monthly, in-situ simulated cases, engaging ED and trauma teams, including fellows, residents, midlevel providers, and nurses. Post-case debrief sessions and participant feedback were complemented by the trauma team and T-NOTECHS evaluations. Simultaneously, we analyzed video recordings of ED trauma cases, employing the same tools for comprehensive assessment. A comparative analysis between the pre-and post-implementation periods was performed, focusing on crucial time-to-intervention metrics.
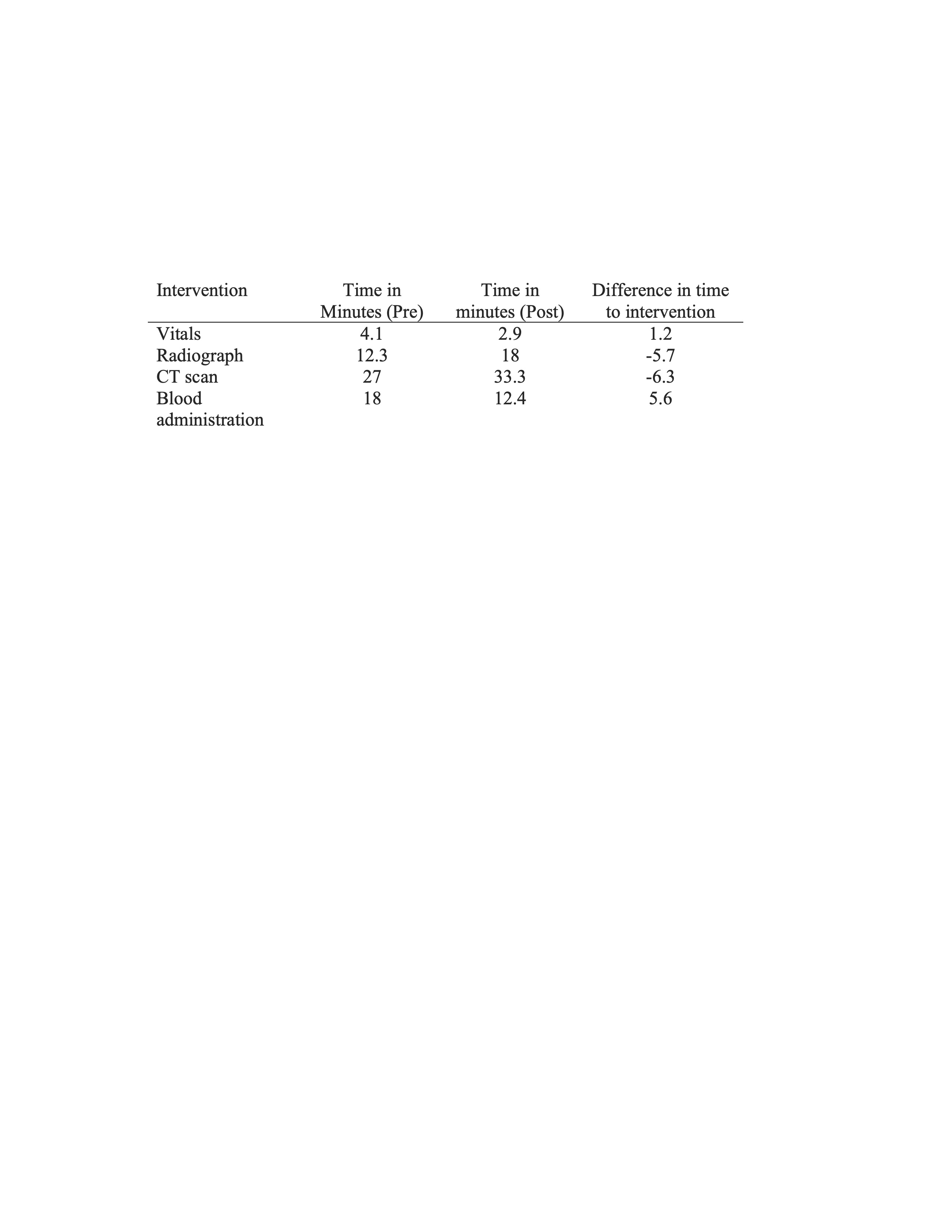
Results: Throughout the study, 14 simulation cases were executed, alongside video review of 248 ED trauma cases, involving the active participation of over 50 trauma personnel. Post-intervention, a marked improvement in trauma team effectiveness was observed, with an increase in average score from 6.7 to 7.4, alongside enhanced performance in key metrics, such as time to vitals and blood administration. Notably, the study recorded a 12% increase in the average T-NOTECHS score, reflecting a significant enhancement in teamwork and communication dynamics within the trauma team.
Conclusion(s): This study highlights the efficacy of low-fidelity interdisciplinary simulations in fostering effective teamwork and addressing critical challenges pertaining to the quality and safety of trauma care. The integration of real-time trauma code video reviews facilitated the evaluation of adherence to standardized protocols and the identification of specific areas for continuous improvement, thereby contributing to an overall elevation in the effectiveness of trauma care in the ED.