Quality Improvement/Patient Safety
Session: Quality Improvement/Patient Safety 4
24 - Improving Febrile Seizure Classification and Documentation to Provide High Value Care and Reduce Variability in Patient Care: A QI Project
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 24
Publication Number: 24.3286
Publication Number: 24.3286
- FS
Farimah Shariati, MD (she/her/hers)
Pediatric Hospital Medicine Fellow
Akron Children's Hospital
Akron, Ohio, United States
Presenting Author(s)
Background: Febrile seizures (FS) are the most common convulsive events in children. The American Academy of Pediatrics classifies FS as simple (SFS) and complex (CFS). SFS are benign events with only a 2% risk of developing into epilepsy, as opposed to CFS which have a 6-8% risk of developing into epilepsy in future. Specific risk factors associated with FS that develop into epilepsy include seizures with focality and ≥ 3 seizures in 24-hours. Correct categorization of FS into SFS or CFS can help reduce variability in care of patients presenting with FS. Further, recognizing high risk features in CFS can help recognize patients in need of further diagnostic workup.
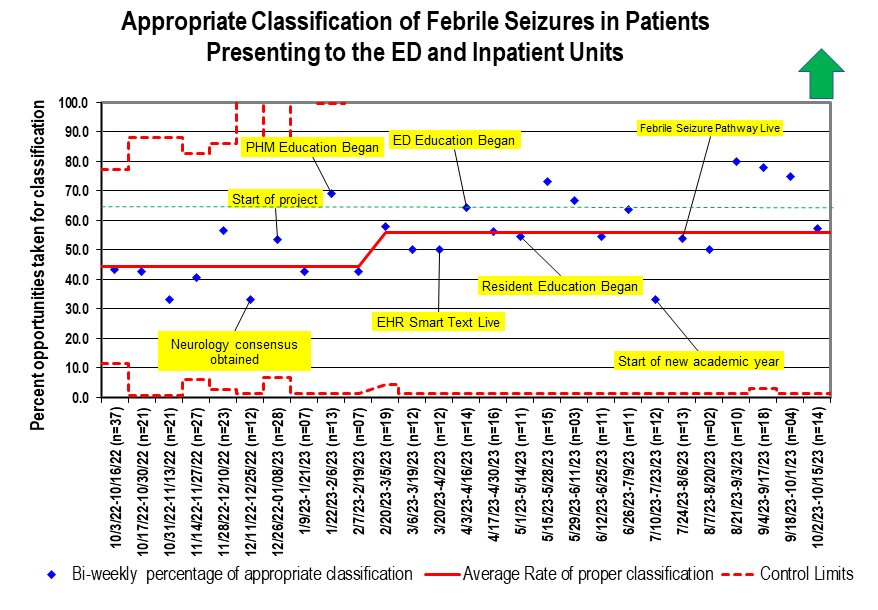
Objective: The aim of this project was to increase documentation of appropriate classification of SFS and CFS from a baseline of 45% to 65 % in 12 months.
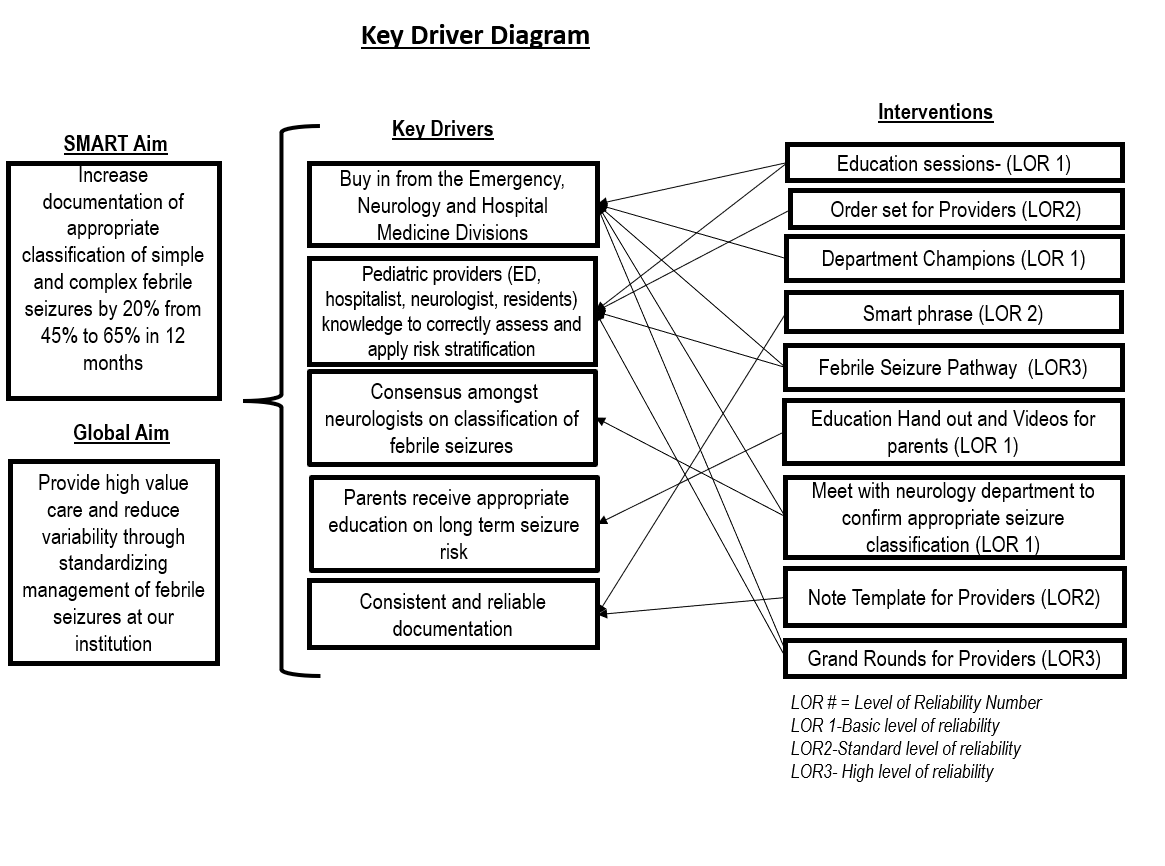
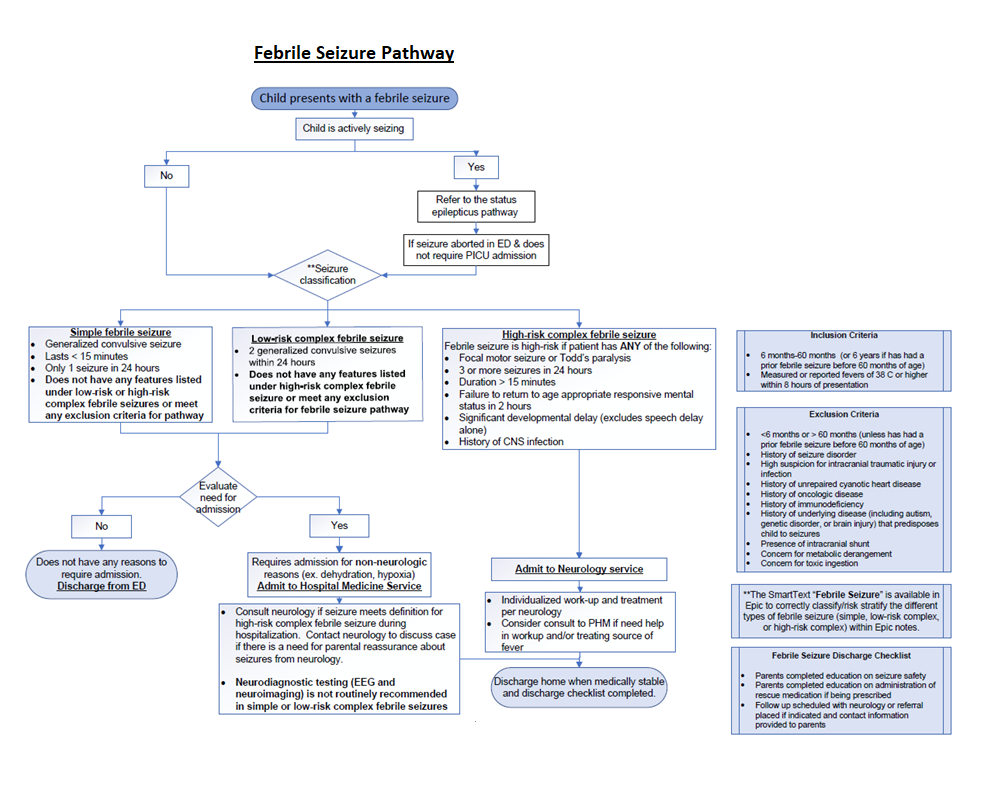
Design/Methods: Model for Improvement was chosen as the QI methodology. After process mapping and literature review a Key Driver Diagram (Fig.1) was created. The primary measure was the percentage of appropriate classification of FS measured biweekly for all patients seen in the ED or admitted to the hospital with ICD Codes of R56.0 (SFS) and R56.01 (CFS). Appropriate classification was defined as provider documentation of either SFS, low risk CFS, or high risk CFS in the electronic health record (EHR). Data was pulled electronically, and manual chart reviews were conducted for all ED encounter and admission notes. Interventions included division specific provider education, obtaining buy-in from various divisions through department champion representation, and creation of a FS pathway (Fig. 2), as well as EHR incorporated smart text for assistance with proper classification.
Results: Our baseline percentage of appropriate classification of FS was 45%. Two months after the start of our project we had a shift indicating a special cause variation with an increase in correct classification of FS from baseline of 45% to 59 % (Fig.3).
Conclusion(s): Although we have not reached our goal of 65%, our interventions have led to some noticeable changes. Future interventions will include ongoing provider education with a focus on new hire providers, addressing further barriers to documentation, and exploring innovative solutions within the EHR, such as creating disease-specific note templates.