Hypertension
Session: Hypertension
66 - Clinician response after receipt of abnormal ABPM – characteristics associated with inertia and action
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 66
Publication Number: 66.1734
Publication Number: 66.1734

Evelien van Gelderen, BA (she/her/hers)
Medical Student
Johns Hopkins University School of Medicine
Baltimore, Maryland, United States
Presenting Author(s)
Background: Ambulatory Blood Pressure Monitoring (ABPM) is recommended to confirm hypertension (HTN). Few studies have investigated factors leading to physician action after receipt of abnormal findings.
Objective: We aimed to identify patient characteristics associated with physician action.
Design/Methods: This was a retrospective cross-sectional analysis of patients 5-22 years of age evaluated in a Johns Hopkins pediatric nephrology clinic who underwent 24hr ABPM between 2003-2022, met criteria for masked or ambulatory HTN, and had a clinic visit within 2 weeks of ABPM. Patient characteristics from the first eligible ABPM/clinic visit were obtained via chart review. “Action” was defined as any combination of medication change/initiation, lifestyle or adherence counseling, evaluation ordered, or interpretation with no change. Characteristics of children with/without physician action were compared using Student t tests with unequal variances and Chi square as appropriate. Multivariable regression analyses were conducted to determine if age, obesity status, or kidney disease was associated with physician action.
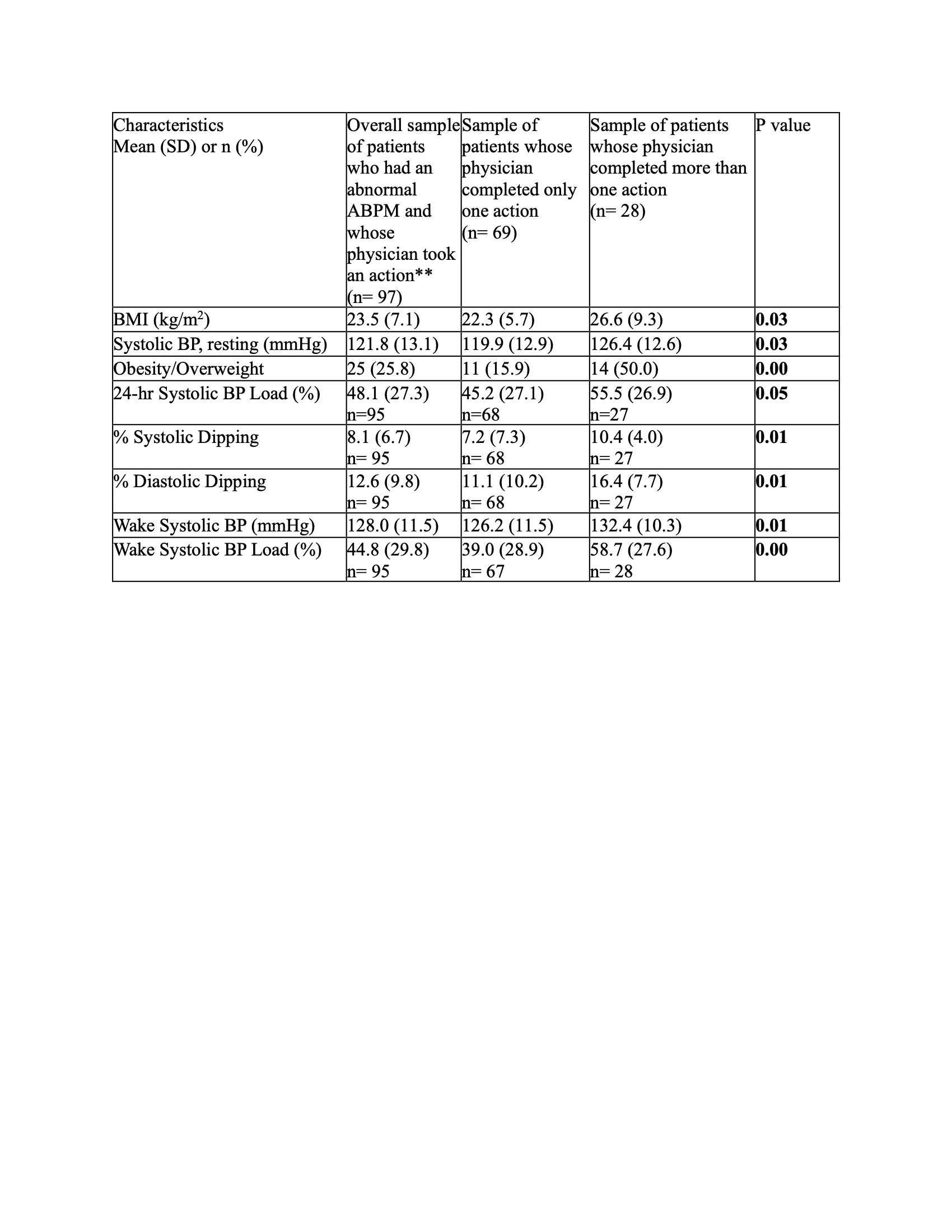
Results: 115 unique patients with masked (n=53) and ambulatory (n=62) HTN were included. The mean age was 13.0 yrs (SD 4 yrs); 48% were female and 38% were of Black race. 24 (21%) had kidney disease; 5 (4%) were undergoing dialysis and 10 (9%) were kidney transplant recipients. 97 (84%) of the encounters had a documented physician response. The most common responses were medication change (46%), evaluation ordered (37%), and prescribed lifestyle change (32%). Adherence counseling was documented in 3% of encounters. Of the 18 patients without action, 67% had masked HTN and 33% had ambulatory HTN. 24-hr and wake SBP load as well as sleep DBP load were significantly higher among those with a physician action than without (Table 1). Patients with >1 action had greater adiposity, greater SBP (resting, wake, load), and greater dipping (Table 2; significant results only). Neither age, obesity, nor kidney disease were independently associated with physician action (data not shown).
Conclusion(s): In this cohort of pediatric patients referred for subspecialty care, 16% of abnormal ABPMs did not have a documented action in response. Characteristics associated with response included greater BP load, and characteristics associated with >1 response included adiposity, higher SBP, and greater dipping. More work is needed to determine how to optimize clinical care for those with an abnormal ABPM, which is a risk factor for later cardiovascular disease and events.
.jpg)