Emergency Medicine
Session: Emergency Medicine 11: Potpourri
408 - Comparing use of crotalidae-polyvalent immune fab [ovine] vs. observation in management of crotalidae snake envenomation in pediatric patients
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 408
Publication Number: 408.3284
Publication Number: 408.3284

Stephen Rohl, DO
Fellow
University of Tennessee Health Science Center - Memphis
Gulf Breeze, Florida, United States
Presenting Author(s)
Background: Approximately 1,300 children are hospitalized annually in the United States (US) from the pit viper family Crotalidae (Rattlesnakes, Copperheads, Cottonmouths). Morbidity may include skin necrosis, coagulopathy, and rare compartment syndrome. Indications for the use of antivenin, Crotalidae polyvalent immune fab (ovine) vary considerably.
Objective: Some US studies (none RCT) recommend aggressive antivenin utilization for Crotalidae envenomation, while other studies recommend a conservative approach. We compared outcome in these two approaches used at 2 separate children’s hospitals. We hypothesized that deferring antivenin leads to increased morbidity and increased hospital length of stay.
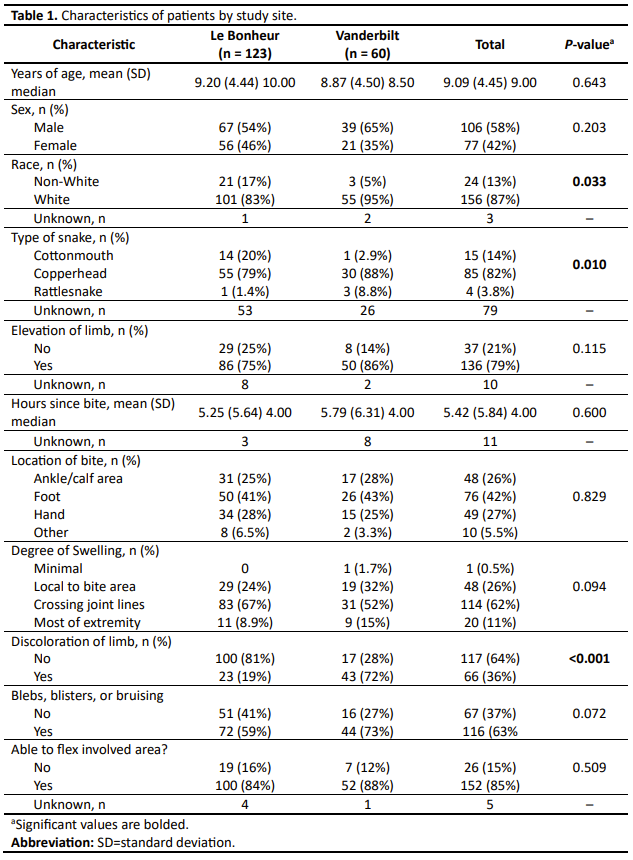
Design/Methods: We performed a retrospective chart review of children who presented to Le Bonheur Children’s Hospital (LBCH) in Memphis, Tennessee and Monroe Carell Jr. Children’s Hospital at Vanderbilt (MCJCHV) in Nashville, Tennessee from 2009–2021 Charts were identified by ICD-9 and ICD10 codes related to snake envenomation. The state Poison Center database was also cross-referenced. A standardized data collection form was created for use at both sites. Data on patient demographics, antivenin utilization, bite location, and outcomes were statistically compared.
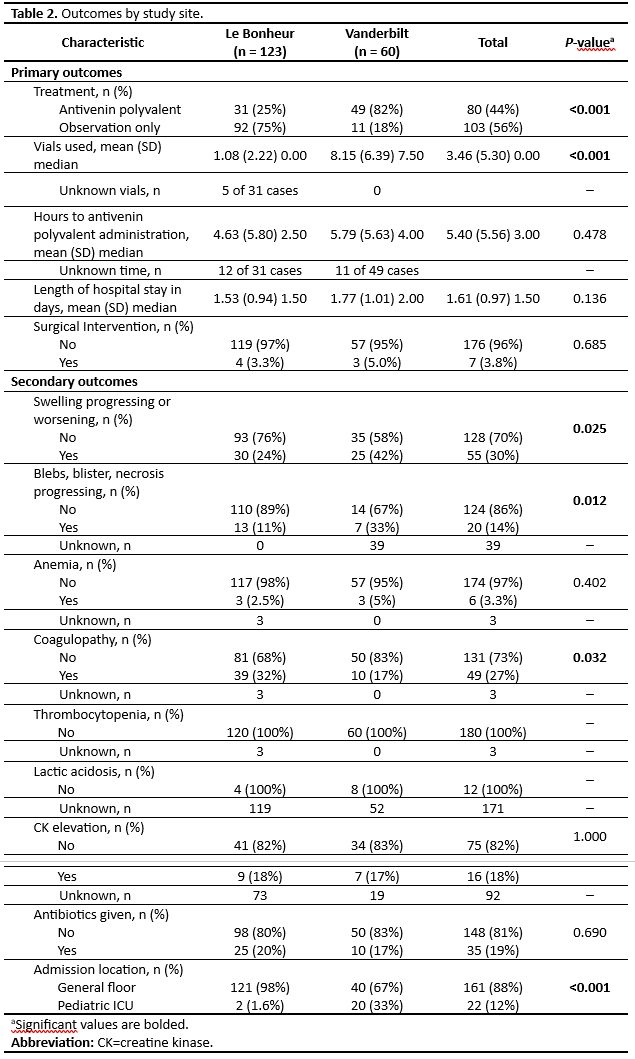
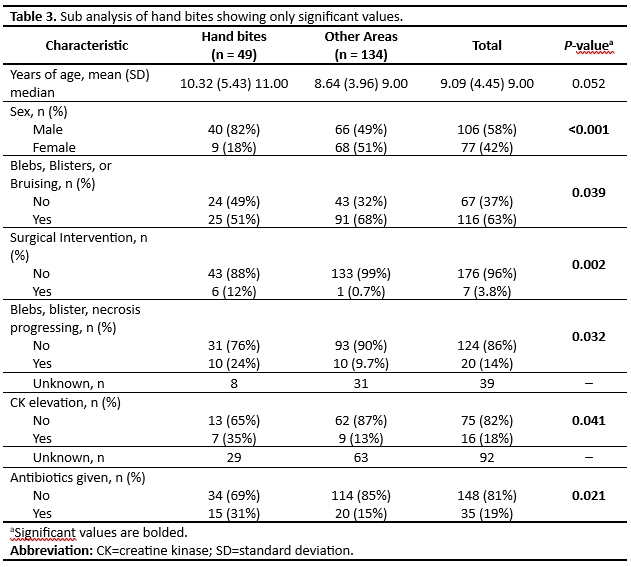
Results: A total of 183 patients met inclusion criteria (123 at LBCH, 60 at MCJCHV). At LBCH, mean age was 9.2 years, and 79% of snakes were identified as copperheads. At MCJCHV, mean age was 8.87 years, and 88% of snakes were identified as copperheads. The most commonly envenomated areas for both sites was the foot (42%), hand (27%), and ankle (26%). Patients at LBCH were managed with antivenin only 25% of the time while 75% were observed; 82% of MCJCHV patients were managed with antivenin (P < 0.001). There were no significant differences in Length of Stay (mean 1.53 days at LBCH, 1.77 days at MCJCHV, P=0.136) or Surgical Intervention (3.3% of LBCH encounters, 5.0% of MCJCHV encounters, P=0.685). Secondary outcomes aside from coagulopathy and admission location (ICU vs. floor) were also not significant.
Conclusion(s): In this retrospective study, antivenin use did not impact hospital length of stay or surgical interventions. Our results are not generalizable in the US as our study reflects regional experiences with snake species in the southeastern US. Additionally, the retrospective nature of this study could have impacted the available data for analysis compared to a large, controlled prospective study. Further prospective study is needed to determine long-term outcomes of deferring antivenin use.