Neonatology
Session: Neonatal Quality Improvement 2
402 - Increasing Enteral Feeding During Therapeutic Hypothermia for Hypoxic-Ischemic Encephalopathy: An Evaluation of Sustainability
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 402
Publication Number: 402.1741
Publication Number: 402.1741
- EL
Emily Lo, MD
Neonatal-Perinatal Medicine Fellow
The Hospital for Sick Children / University of Toronto
Toronto, Ontario, Canada
Presenting Author(s)
Background: Historically, enteral feeding during therapeutic hypothermia (TH) was withheld due to concerns of gut hypoperfusion and potential association with feeding intolerance. Recently studies have shown that enteral feeding during TH is safe and associated with higher breastfeeding rates and shorter NICU length of stay.
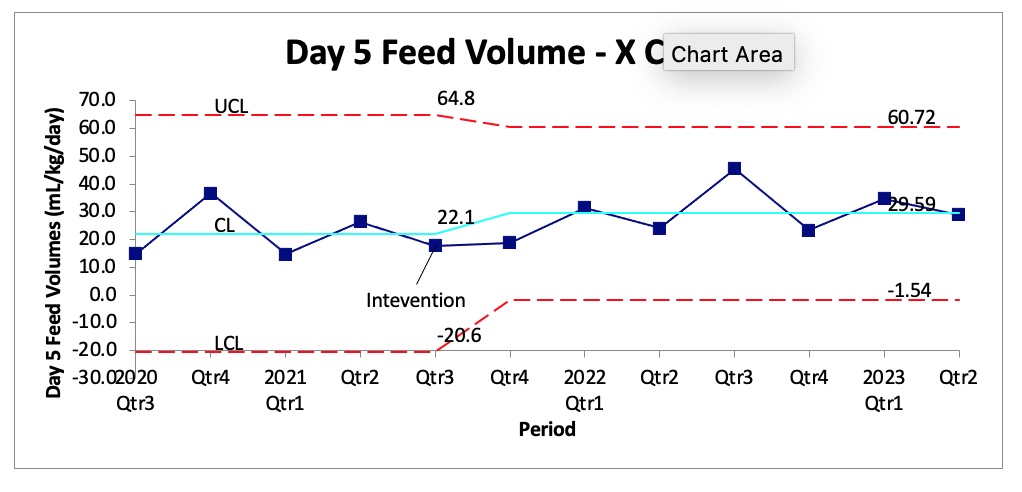
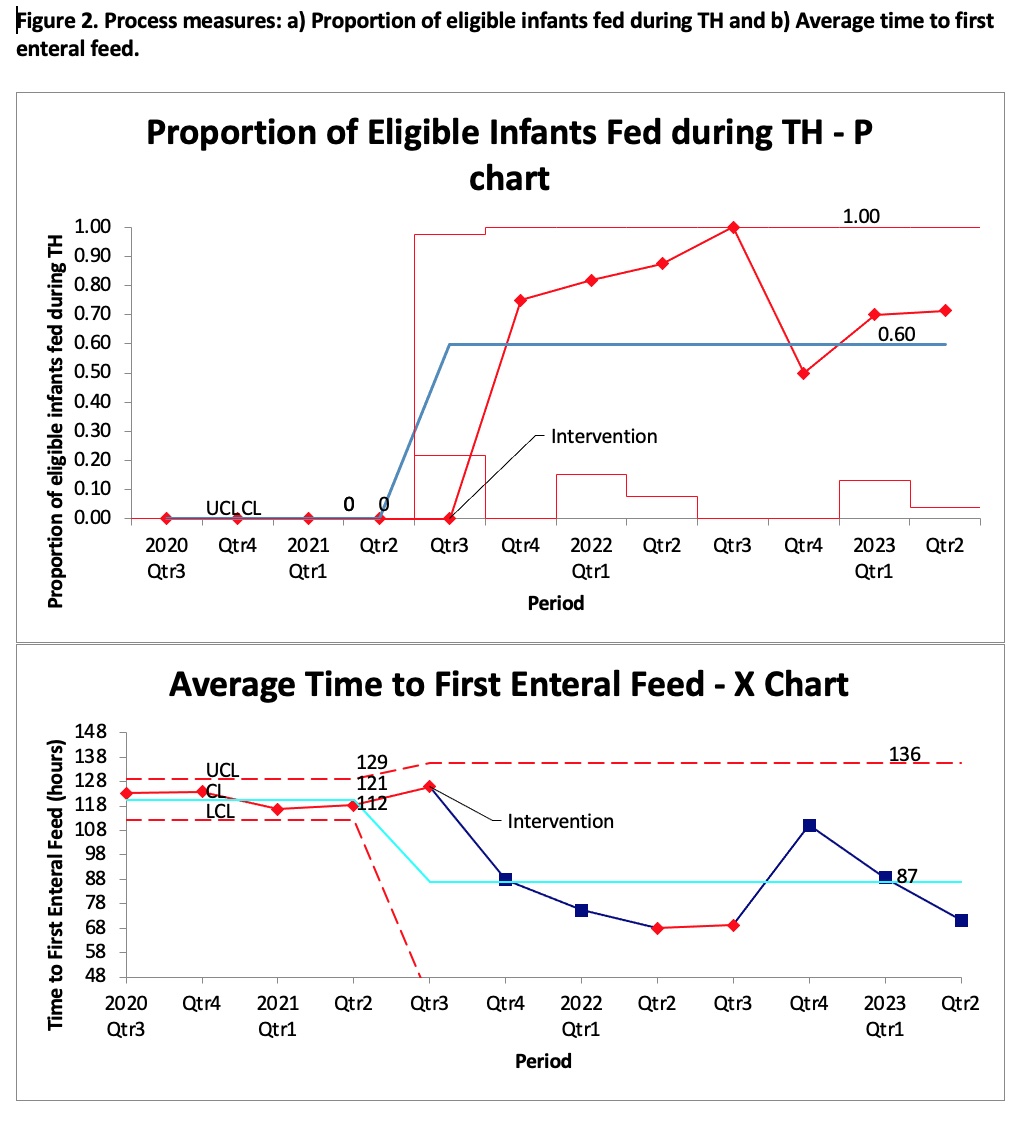
Objective: To evaluate the sustainability of increasing day five enteral feeding volumes for eligible infants undergoing TH from September 2021 to June 2023, after the introduction of new feeding guideline in September 2021, in the NICU of a large academic hospital.
Design/Methods: In this quality improvement (QI) project, we used the Plan-Do-Study-Act (PDSA) methodology, process mapping and fishbone analysis. We implemented interventions including the development of clinical practice guidelines to promote early enteral feeding during TH and teaching sessions with interprofessional groups.
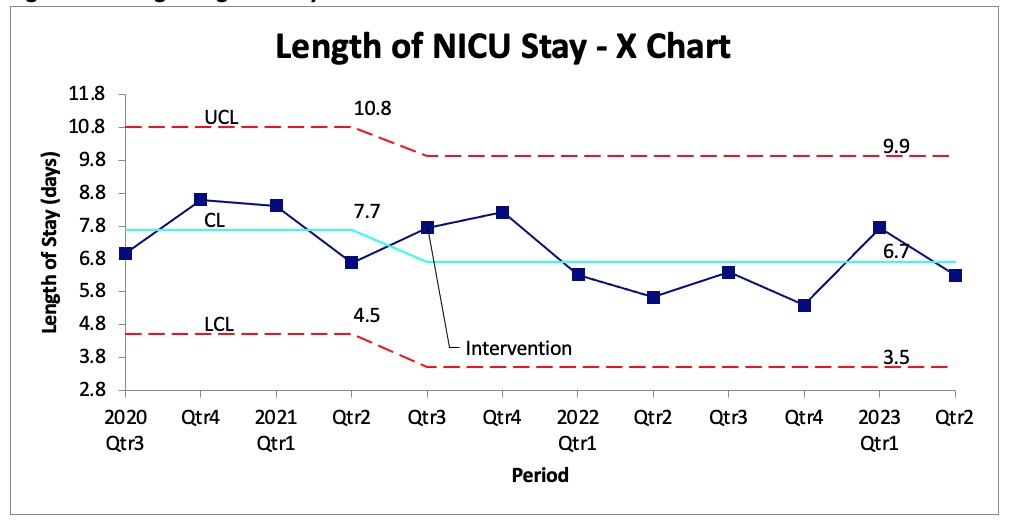
Results: We evaluated 41 and 61 neonates pre- (Sept 2020-Aug 2021) and post-intervention (Sept 2021-June 2023), respectively. The outcome measure was day five feed volumes, which was 22.1 mL/kg/day and 29.6 mL/kg/day, pre and post respectively (p=0.26) (Figure 1). The process measure was proportion of eligible infants fed during TH which was 60% in the postintervention period and time to first enteral feeds which decreased from 121 hours to 87 hours, pre and post respectively (p < 0.01) (Figure 2). Median length of NICU stay decreased from 7.7 days to 6.7 days (p=0.26) (Figure 3). The balancing measure was incidence of feeding intolerance, where there was 1 case pre-intervention and 0 cases post-intervention.
Conclusion(s): Using QI methods, we implemented enteral feeding in the majority of eligible infants and decreased time to first feed without increasing the incidence of feeding intolerance. Additional PDSA cycles to increase compliance with the feeding guideline are planned.