Quality Improvement/Patient Safety
Session: Quality Improvement/Patient Safety 4
21 - Early HPV Vaccine Uptake Through the Lens of Health Disparities: A QI Initiative to Increase HPV Vaccine Uptake Prior to 11 Years Old
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 21
Publication Number: 21.3275
Publication Number: 21.3275
.jpg)
Caitlin J. Miller, BA (she/her/hers)
Medical Student
Sidney Kimmel Medical College at Thomas Jefferson University
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: HPV vaccine is effective in preventing HPV-related cancer. Routine HPV vaccination starts at 11 y.o. Early initiation at 9 and 10 y.o increases HPV vaccine uptake, which remains lower than other childhood vaccinations. Incidence of HPV-associated cervical cancer is higher for both rural and black patients, highlighting disparities in care. Nemours Children’s Health Delaware Valley primary care network serving 130,000 children embarked on a multi-year quality improvement (QI) project to improve HPV vaccine uptake with early initiation.
Objective: Analyze trends in early HPV initiation by race/ethnicity, geography, insurance, and child opportunity index (COI).
Design/Methods: Using QI methodology we developed a multi-pronged approach to improve early initiation of HPV vaccine. Primary outcome measure was HPV HEDIS measure, defined as the proportion of active primary care patients fully vaccinated for HPV by 13 y.o. The process measure was the proportion of active primary care patients 9 and 10 y.o with early initiation of HPV vaccine. Year-end vaccine initiation rates prior to 11 y.o were analyzed to assess trends by race/ethnicity, geography, insurance, and COI.
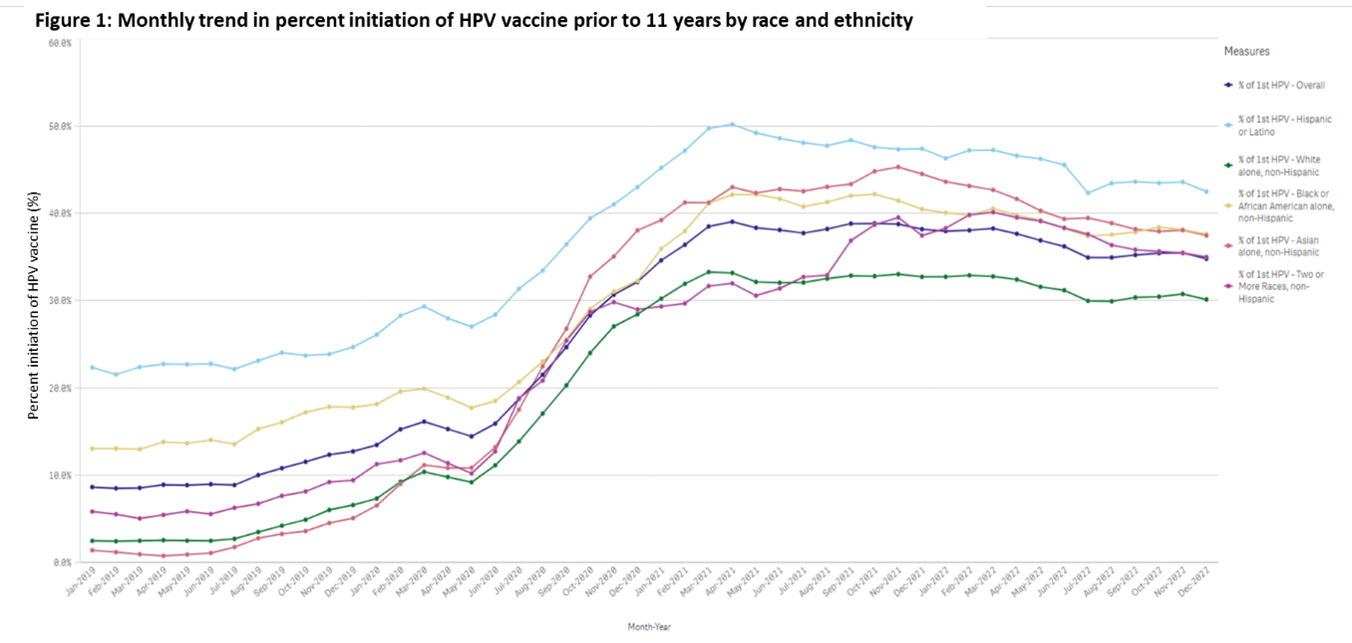
Results: HPV HEDIS rate improved annually from baseline of 49.2% in 2019 to 59.5% in 2022 (p < 0.0001). Early HPV initiation improved overall from a baseline of 12.7% in 2019 to 34.8% in 2022 (p < 0.0001). Early HPV initiation improved significantly from 2019 to 2022 (p < 0.0001) for each racial/ethnic group (Fig. 1 & 2). The proportion of Medicaid patients with early HPV initiation increased from 19.5% in 2019 to 46.2% in 2022 (p < 0.0001) and 8.8% to 39.9% (p < 0.0001) for non-Medicaid patients. The proportion of rural patients with early HPV initiation increased from 1.8% in 2019 to 33.1% in 2022 (p < 0.0001), and for urban patients 13.7% in 2019 to 42.7% in 2022 (p < 0.0001). Early HPV initiation increased from 2019 to 2022 in patients of all COI levels (Table 1).
Conclusion(s): QI efforts to increase early HPV initiation prior to 11 y.o were effective across all patient populations, regardless of race, ethnicity, COI or insurance status. By 2022, the highest rate of early HPV initiation was observed in the lowest COI patient population and in patients who identified as Hispanic or Latino. This multi-pronged QI approach was instrumental in increasing early HPV initiation in populations with the lowest HPV rates in 2019, such as rural, Asian, White, and non-Medicaid insured patients.