Nephrology
Session: Nephrology 2
24 - Post-Transplant Lymphoproliferative Disorder in Pediatric Kidney Transplant Patients
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 24
Publication Number: 24.1609
Publication Number: 24.1609
- SR
Shannon Reinert, MD (she/her/hers)
Fellow
Cincinnati Children's Hospital Medical Center
Cincinnati, Ohio, United States
Presenting Author(s)
Background: Post-transplant lymphoproliferative disease (PTLD) is a rare but potentially serious complication after kidney transplantation. PTLD is a heterogenous disease, more common in children, and with variable presentations and treatment approaches.
Objective: This study describes the presentation, treatment, and outcomes of PTLD in the kidney transplant (KT) population at a large midwestern pediatric KT center.
Design/Methods: Retrospective chart review of pediatric KT recipients who subsequently developed PTLD. All KT patients who received post-transplant care from January 1, 2010 to June 30, 2023 at Cincinnati Children’s Hospital Medical Center were included. Data for baseline characteristics, recipient and donor EBV status, induction therapy, type of PTLD, time to PTLD diagnosis, treatment, and therapy response were extracted.
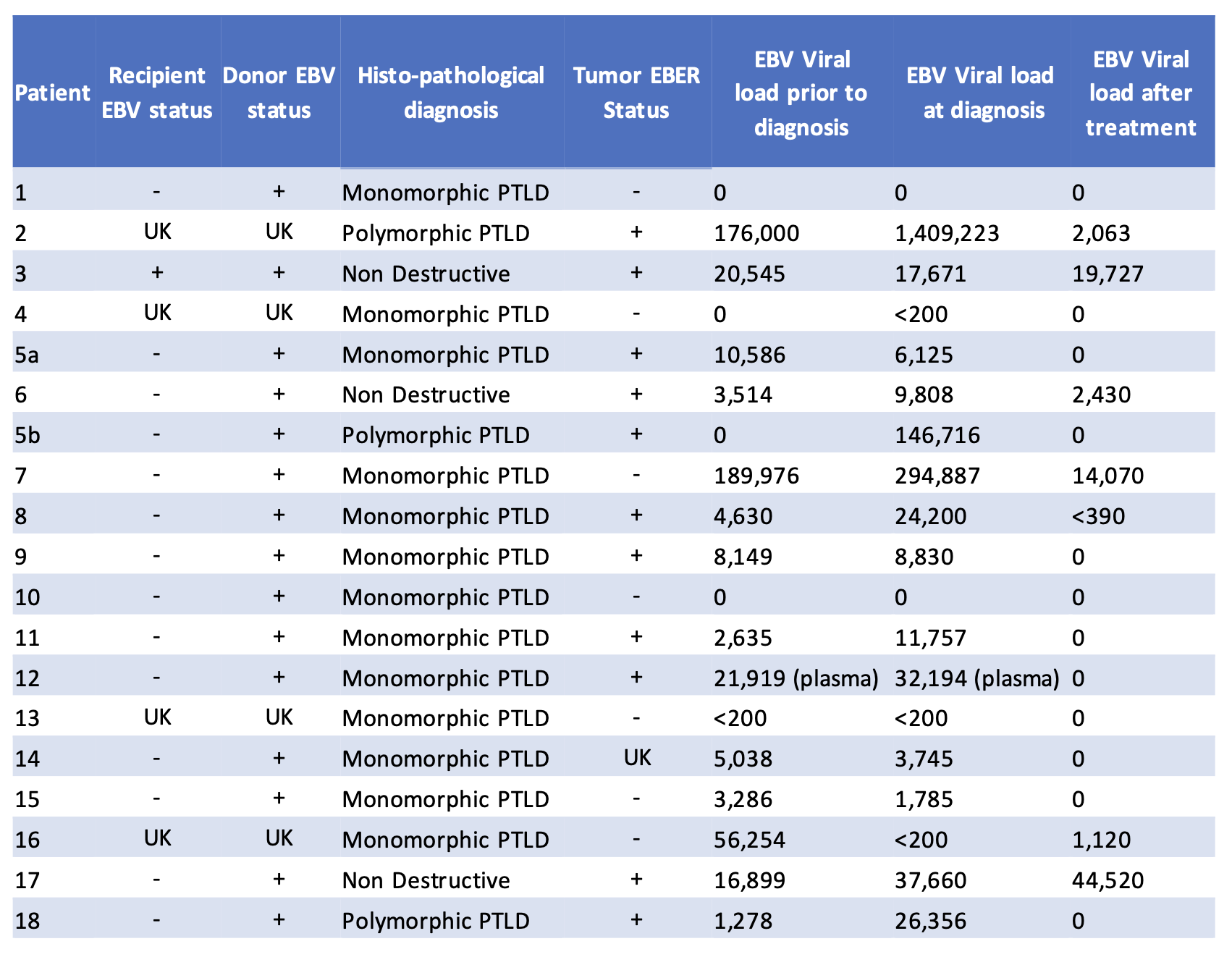
Results: 18 patients were identified with PLTD. One patient had 2 morphologically unique cases of PTLD, which were treated as 2 unique cases. Mean age at diagnosis was 11 years (SD 5 years). Median time to diagnosis was 3.7 years (IQR 0.5-8.25). 9 cases were within 2 years of transplant (Early PTLD), 6 were 2-10 years after transplant (Late PTLD), and 4 were over 10 years after transplant (Very Late PTLD). 14 patients were Epstein-Barr virus (EBV) donor+/recipient-, 1 was donor+/recipient+, and 4 were unknown. Symptoms leading to PTLD work-up included EBV viremia (8 cases), fever (6), gastrointestinal symptoms (7), tonsillar hypertrophy (2), and lymphadenopathy (5). Lesions were subclassified as non-destructive (3 cases, all EBER positive), monomorphic PTLD (7 EBER negative, 5 EBER positive, 1 EBER unknown), and polymorphic PTLD (All EBER positive). Initial therapy included reduction in immunosuppression alone (4 cases), Rituximab/Obinutuzumab (R/O) alone (5 cases), chemotherapy (2 cases), or chemotherapy and R/O (8 cases). 3 patients had recurrence requiring additional therapies. Although 5 patients lost their graft by time of analysis, graft failure was not attributed to PTLD in any patients. No patient deaths were attributed to PTLD.
Conclusion(s): The clinical presentation for PTLD was highly variable. Although there is a strong association between EBV and PTLD, many cases were not associated with EBV. Treatment depends on morphologic subtype. Non-destructive lesions occur early, are EBV driven, and often respond to reduction in immunosuppression alone. EBV negative PTLD was more common in patients further out from transplant, all of whom received chemotherapy. This study further highlights the heterogenous nature of PTLD.
.png)
.png)
