Neonatology
Session: Neonatal Quality Improvement 2
404 - Optimizing respiratory management to reduce bronchopulmonary dysplasia in preterm infants: A quality improvement initiative
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 404
Publication Number: 404.1748
Publication Number: 404.1748

Katherine Coughlin, MD (she/her/hers)
Attending Neonatologist
Sharp Mary Birch Hospital for Women and Newborns
San Diego, California, United States
Presenting Author(s)
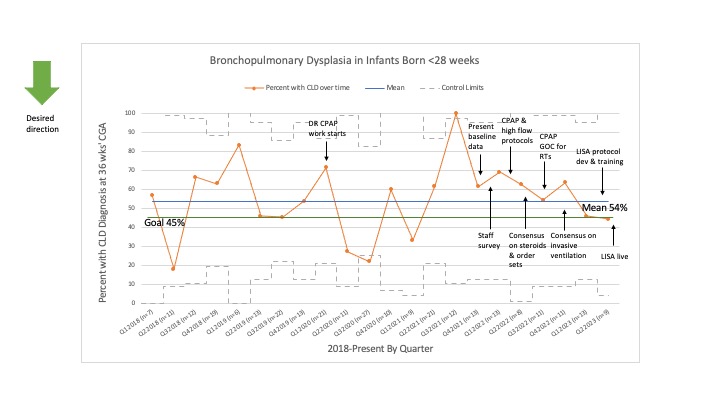
Background: Preterm infants often require intubation and mechanical ventilation, however ventilator days are associated with an increased risk of bronchopulmonary dysplasia (BPD). Minimizing invasive ventilation and optimizing non-invasive ventilation may decrease BPD and improve long term outcomes in preterm infants. For preterm infants born < 28 weeks’ GA at the Sharp Mary Birch Hospital (SMB) NICU, the baseline rate of bronchopulmonary dysplasia (BPD) was 54%.
Objective: Our primary aim was to decrease the incidence of BPD in infants born < 28 weeks from 54% to 45% by June, 2023 at SMB. We sought to achieve this by initially focusing on the following interventions: 1. To decrease the percentage of infants who remain mechanically ventilated at 7 days of life and 2. To decrease the rate of intubation in the delivery room. These became our two process measures.
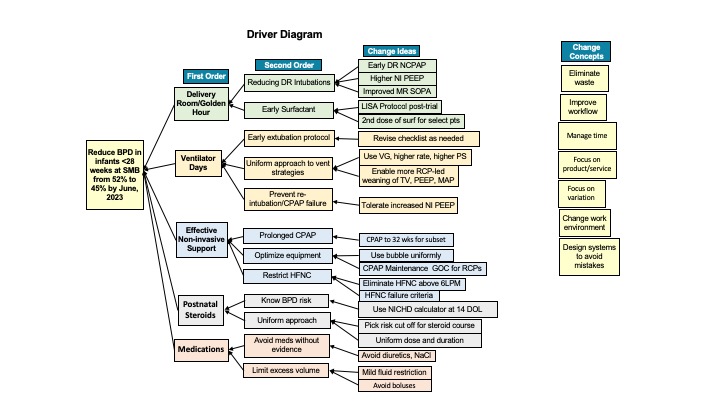
Design/Methods: This was an interdisciplinary quality improvement initiative utilizing the Model for Improvement. A driver diagram was created at project start and modified over time (Figure 1). PDSA cycles included a staff survey to better understand the problem, standardizing the use of bubble CPAP in the delivery room and prolonged CPAP in the unit, reaching consensus on postnatal steroid use, creating guidelines of care for non-invasive management, refining extubation criteria, and building consensus on invasive ventilation strategies. Measures were tracked longitudinally using statistical process control (SPC) charts.
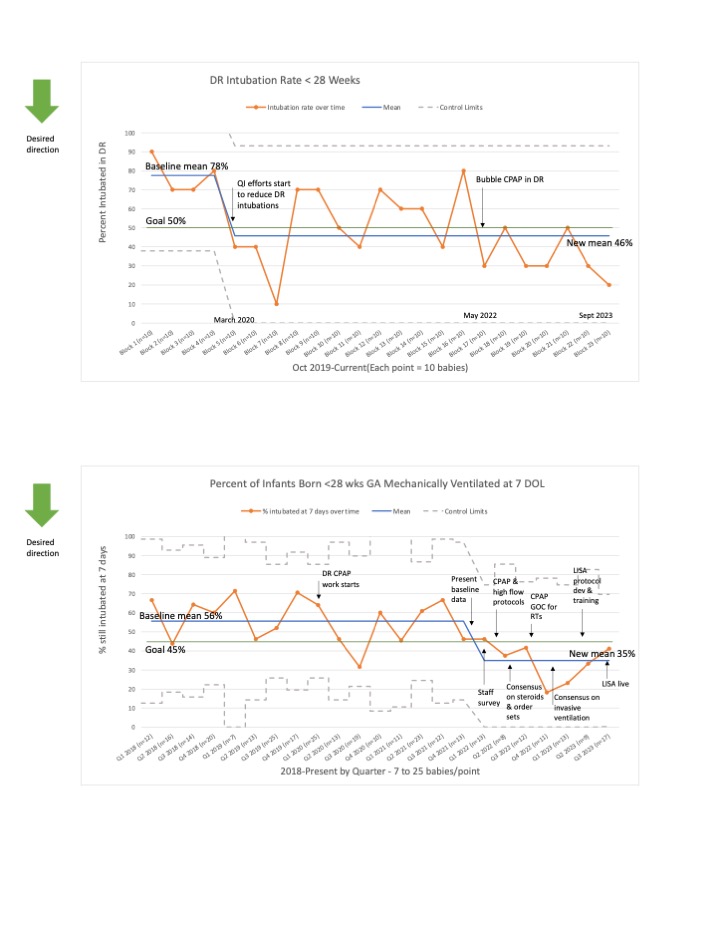
Results: Baseline data collection began in January, 2018. To date, we have included 292 preterm infants born < 28 weeks’ GA. For the process measure of delivery room intubations, we shifted our mean from 78% to 46% on SPC p-chart (Figure 2). For the process measure of infants who remained intubated at 7 days, we shifted our mean from 56% to 35% on SPC p-chart (Figure 2). For the primary outcome of infants with BPD, we have not been able to shift our mean, but met our goal the first two quarters of 2023 (Figure 3).
Conclusion(s): We have implemented multiple evidence-based interventions with the goal of reducing BPD in the SMB NICU for infants born < 28 weeks’ GA. We reduced delivery room intubations by 41% and reduced the percentage of infants intubated at one week by 37%. Our next step is to increase the use of minimally invasive surfactant administration by adoption of a less invasive surfactant administration (LISA) protocol.