Nephrology
Session: Nephrology 2
27 - Social Determinants of Health and Access to Pediatric Kidney Transplantation
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 27
Publication Number: 27.1605
Publication Number: 27.1605
- BF
Brandon M. Fairless, MD (he/him/his)
Fellow
Baylor College of Medicine
Houston, Texas, United States
Presenting Author(s)
Background: Kidney transplantation (KT) is the most effective treatment for patients with end stage kidney disease. Living donor kidney transplant (LDKT) generally results in better outcomes than deceased donor kidney transplant (DDKT). Pre-emptive KT, which allows patients to bypass undergoing maintenance dialysis, is associated with improved patient and graft survival. Studies in the US pediatric population have shown racial disparities in kidney transplant listing and the type of transplant received, but have yet to assess the association between transplant type (LDKT vs DDKT) or access to pre-emptive transplant and socioeconomic status (SES).
Objective: To utilize geocoded data to quantify SES disadvantage and analyze its impact on access to pediatric KT.
Design/Methods: Single-center retrospective chart review was conducted for all pediatric kidney transplant recipients at Texas Children’s Hospital from 2010 to 2022 (n=284). Multi-organ transplantation and re-transplantation were excluded. Transplant type, listing date, and patient address were obtained from UNET transplant registry. Pre-emptive transplant was defined as transplantation prior to initiation of dialysis. Based on patient addresses, neighborhood-level SES disadvantage was categorized using the Area Deprivation Index (ADI) score. ADI scores were calculated based on patient transplant year, and then stratified into quartiles (Q1=least disadvantaged, Q4=most disadvantaged). Differences in characteristics between groups were determined by the chi-square or Fisher’s exact tests for categorical variables and Kruskal Wallis test for continuous variables.
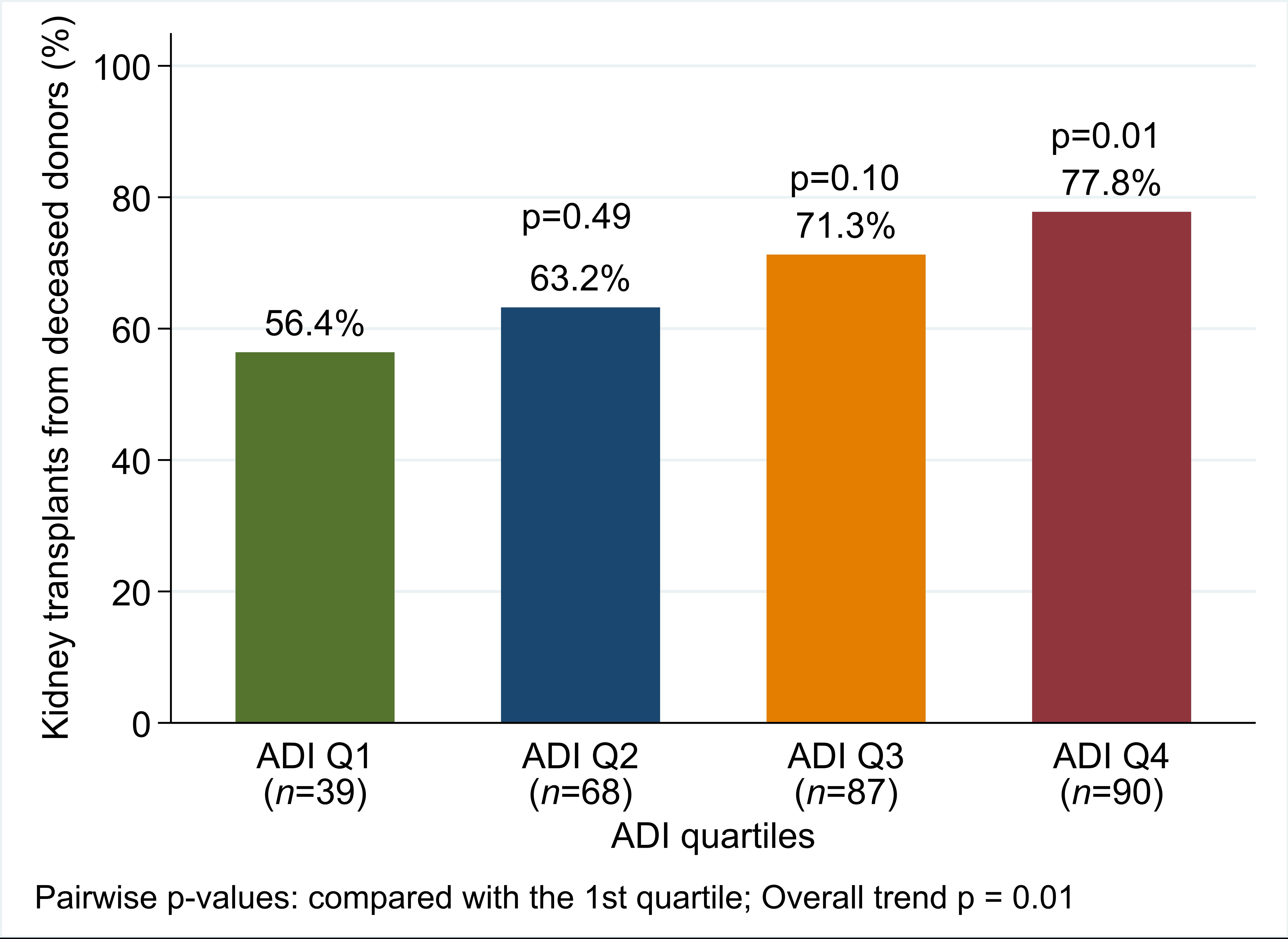
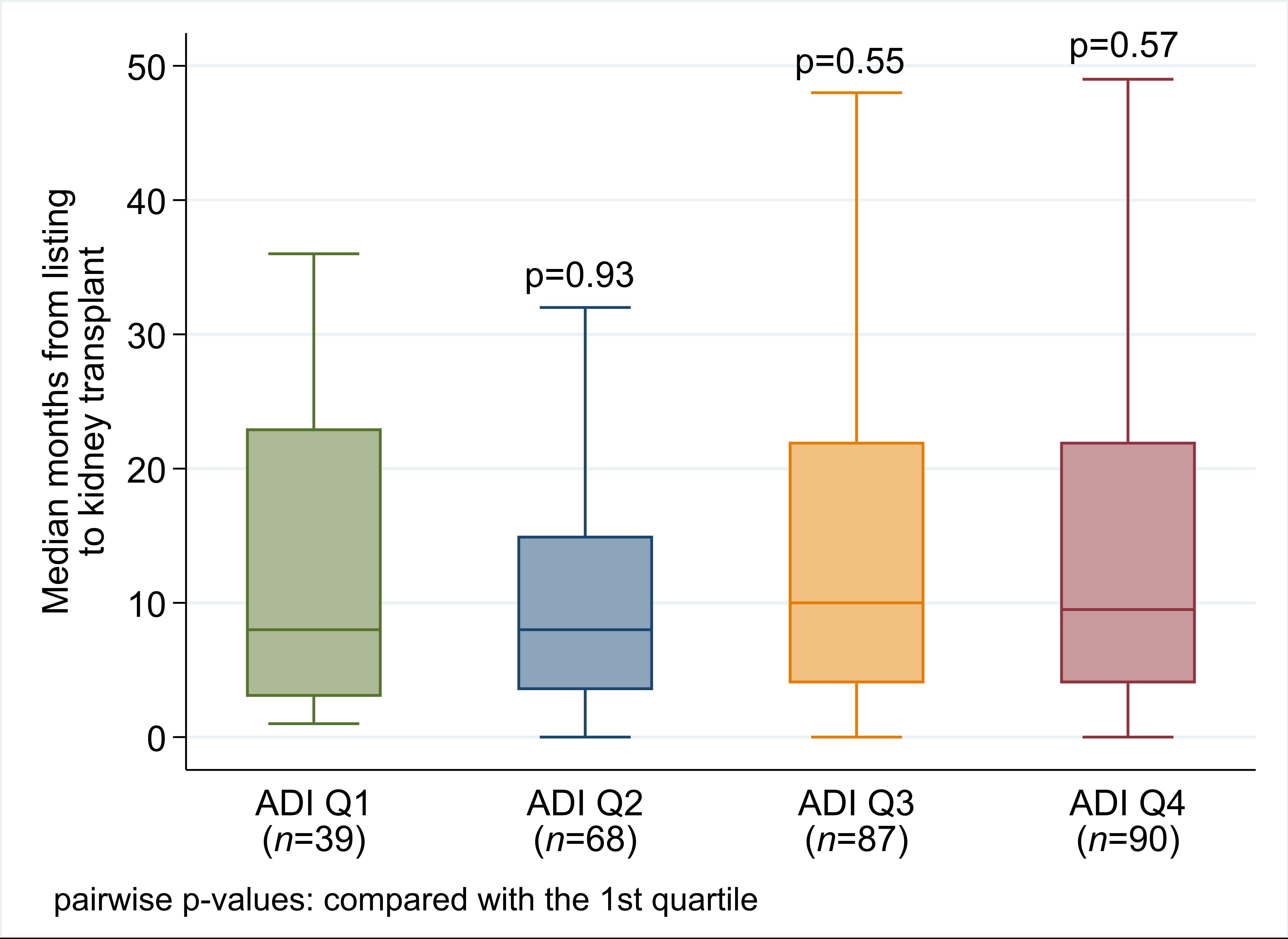
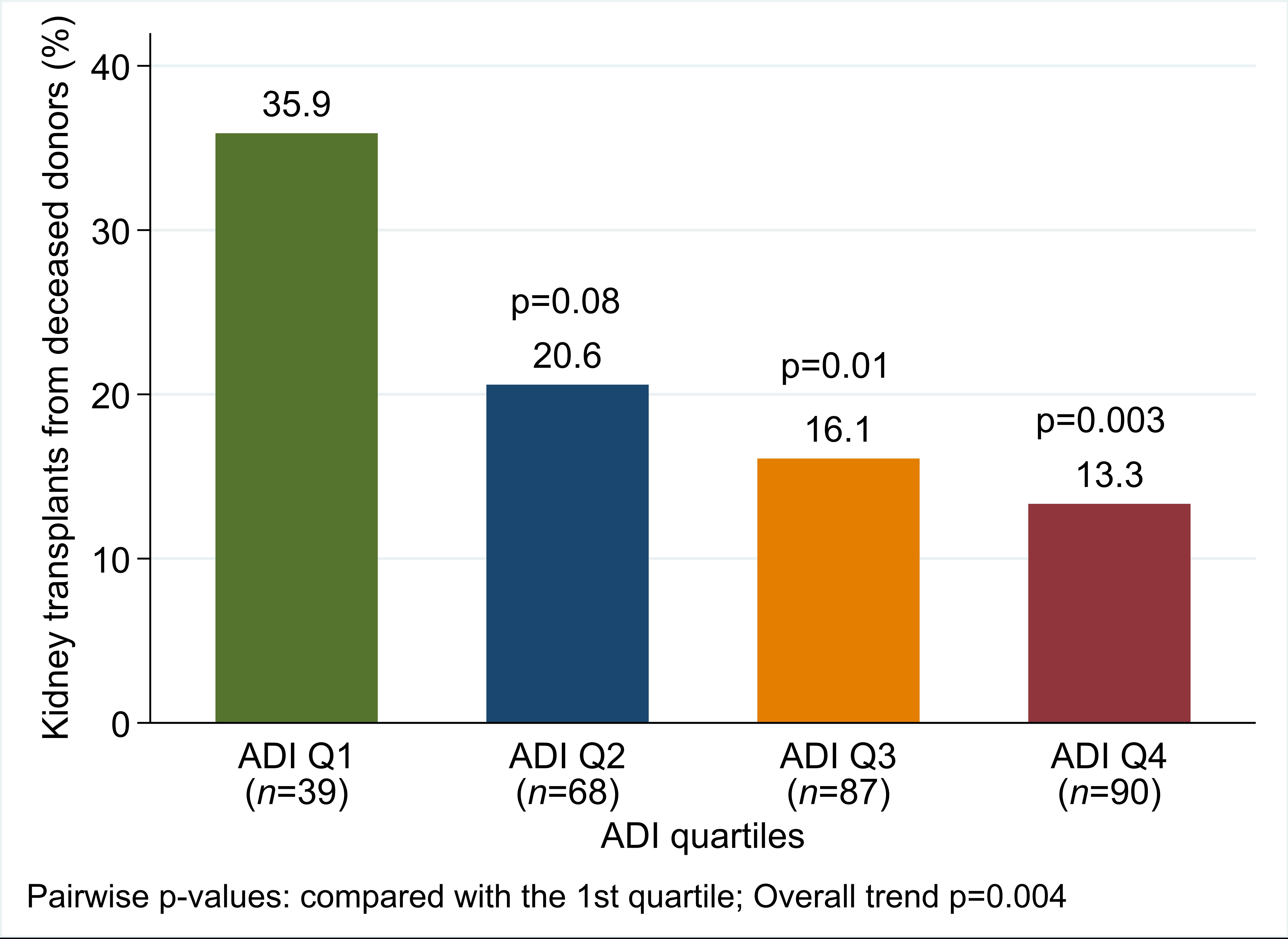
Results: The majority of pediatric patients (62%) who received a KT during the study period resided in the most disadvantaged neighborhoods (Q3 and Q4). There was a significant trend favoring DDKT as ADI quartile increased (Q1=56.4%, Q4=77.8%, p=0.01). Concurrently there was a significant decline in pre-emptive kidney transplant rates as ADI quartile increased (Q1=35.9%, Q4=13.3%, p=0.004). There was no difference in the time from listing to transplant across ADI quartiles.
Conclusion(s): These findings suggest that pediatric KT recipients from socially disadvantaged households were less likely to receive a preemptive transplant or a LDKT. Utilizing geocoded data can provide an objective assessment of patients’ SES that supplements subjective pre-transplant screening tools, which can augment the ability to identify patients at increased risk. There is a need for a targeted approach to expand access to pre-emptive and LDKT for patients living with SES disadvantage.