Neonatology
Session: Neonatal Hematology & Bilirubin Metabolism
456 - Neonatal Transfusions: Will We Continue Accepting this Problem Indefinitely?
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 456
Publication Number: 456.1598
Publication Number: 456.1598

Angela B. Hoyos, MD
Professor
Universidad El Bosque
BOGOTA D.C., Distrito Capital de Bogota, Colombia
Presenting Author(s)
Background: The frequency of packed red blood cells (PRBC) transfusions in premature infants during the neonatal period remains unacceptably high, and efforts to reduce them has been partially ineffective. A recent study from one of our NICUs showed that with the use of erythropoietin, parenteral iron and decreasing the number of phlebotomies, PRBC transfusions can be greatly reduced even when the hemoglobin thresholds guidelines for transfusions is similar compared with other units. (1)
Objective: To review the rate of PRBC transfusions in the EpicLatino Neonatal Intensive Care Units (NICUs).
Design/Methods: EpicLatino is a network of 32 NICUs in Latin American and the Caribbean (see table 1). In this retrospective study we looked at the number of transfused patients ≤ 32 weeks gestational age at birth (GA) during the last 8 years (2015-2022), using Unit 2 as a base with the best results. We sent a questionnaire to update the data on pre-transfusion hemoglobin levels guidelines in units that were not included in the article mentioned in the introduction. We performed a logistic regression controlling for the following variables: GA, necrotizing enterocolitis (NEC), epoch 2015-2019 vs. 2020-2022 (before or during/after the pandemic) and mortality. The information was obtained from the EpicLatino database. For the statistics we used Stata 18, StataCorp LLC, Texas, USA.
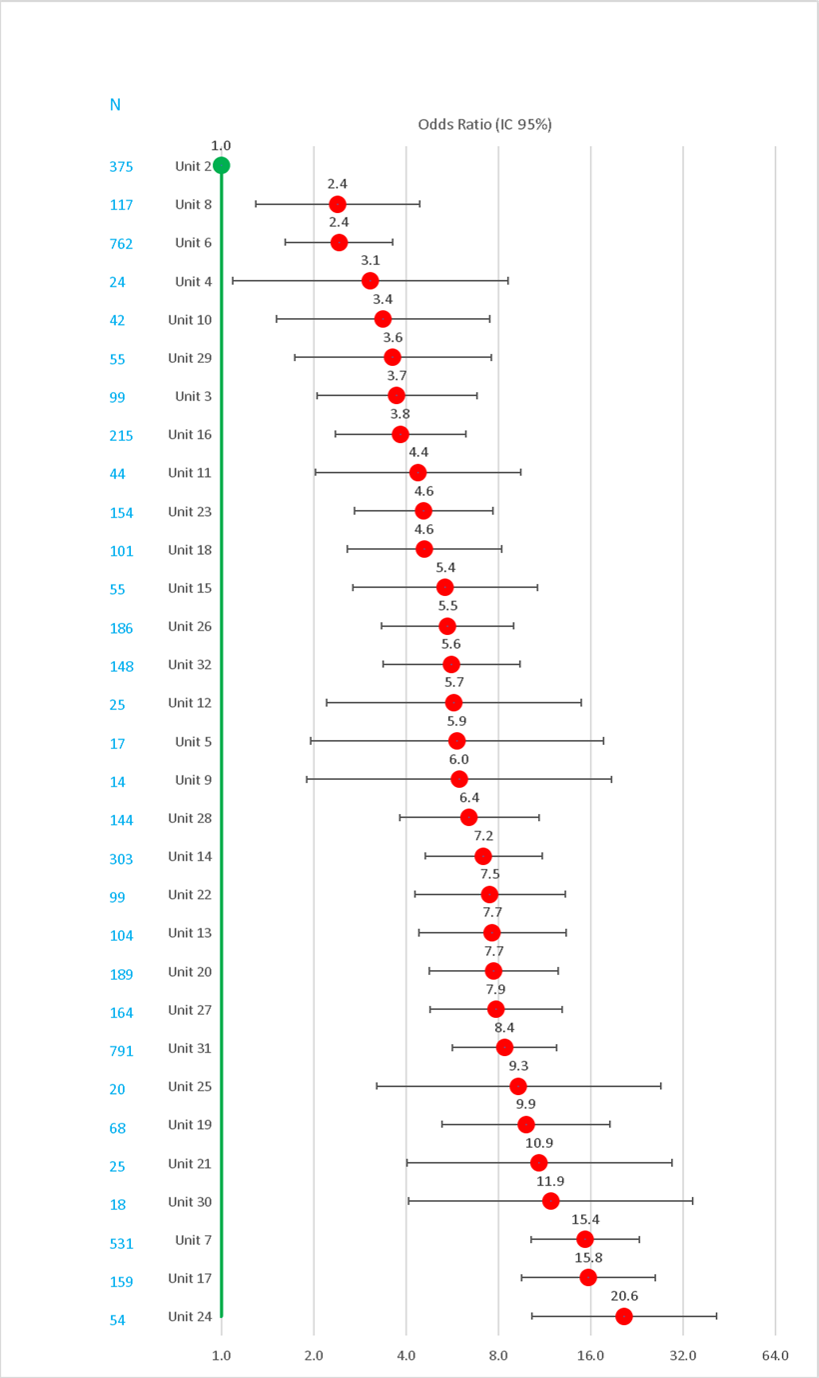
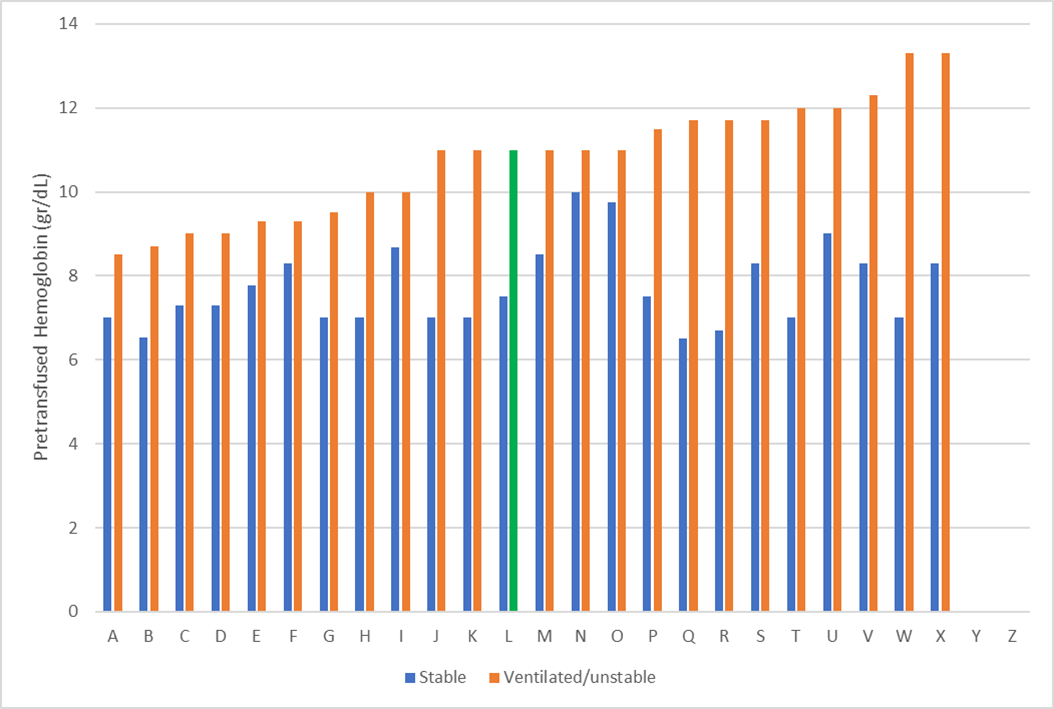
Results: Figure 1 displays the results of the 32 EpicLatino NICUs. The light blue numbers represent number of cases in each unit. The red bars indicate units with a significant difference (all of them) and their 95% confidence interval (CI), while the green bar represents Unit 2 used as the reference. Figure 2 shows the information on average pretransfusion levels guidelines reported by directors in the different EpicLatino Units. In green Unit 2.
Conclusion(s): We are aware of the methodology to prevent transfusions from the unit with the lowest rates (Unit 2), which has been previously published as mentioned. The difference cannot be attributed to pre-transfusion levels by unit 2, as seen in Figure 2.
The noticeable difference between Unit 2 and the other units suggests that the Unit 2 protocol may be useful to prevent transfusions.
1. J Perinatol. 2021:41(6):1403