Technology
Session: Technology 2
189 - From Exam Room to Virtual Reality: Reimagining Pediatric Mental Health
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 189
Publication Number: 189.1766
Publication Number: 189.1766
- JB
Joshua Broadman, MD (he/him/his)
Pediatric Resident Physician
University of Florida College of Medicine
Jacksonville, Florida, United States
Presenting Author(s)
Background: There is a mental health (MH) crisis, especially in adolescents. This vulnerable group suffers from access issues and reluctance to engage with physicians. Evidence shows that virtual reality (VR) enhances communication and rapport between doctors and pediatric patients, though research on physician VR perceptions and usability regarding MH is lacking.
Objective: We conducted a mixed-methods study to evaluate VR as a tool for improving screening and diagnosing adolescent mental health. This pilot study aimed to evaluate the efficiency and usability of a VR clinic app. It also explored physicians’ technological adoption and familiarity with VR in pediatric MH.
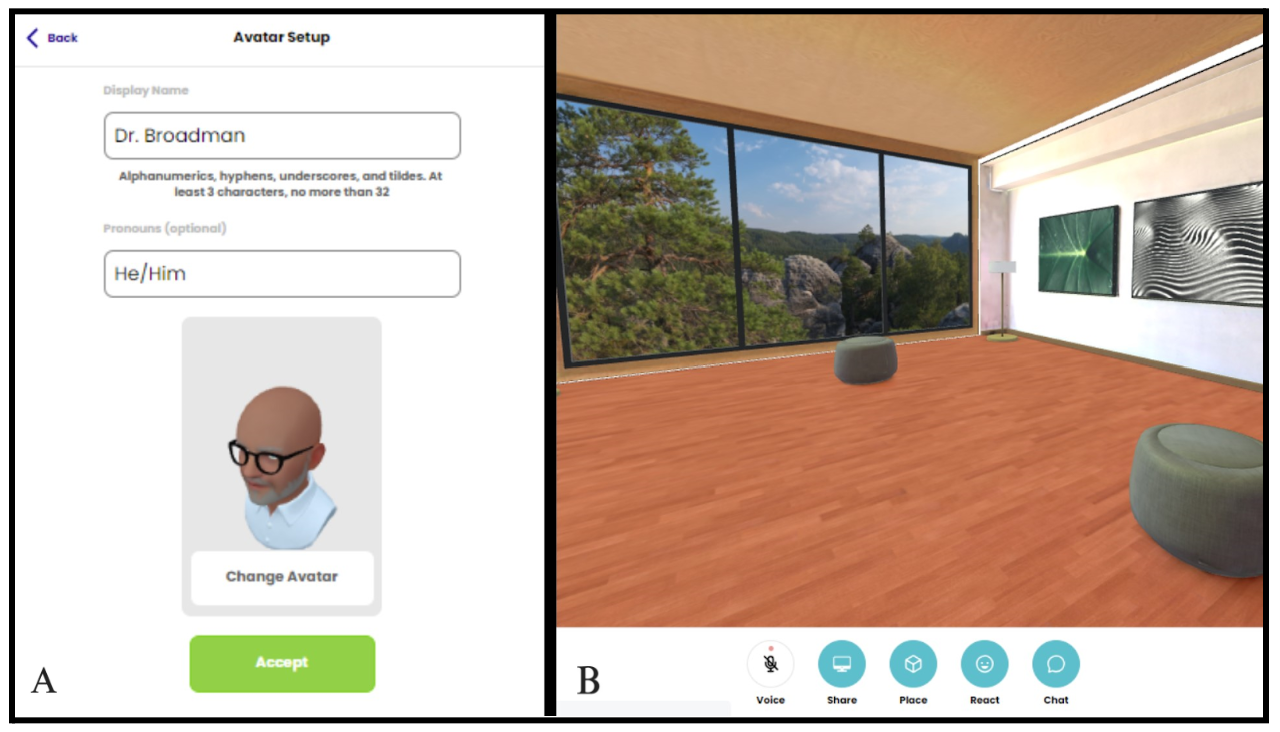
Design/Methods: We recruited 14 pediatric physicians who completed surveys on medical technology, VR usage, and demographics. Participants engaged in a 15-minute structured visit within a VR clinic (Image 1), created in Mozilla Hubs and operated via an Oculus Quest, to diagnose MH issues in a male adolescent portrayed by an actor. Post-study, they filled out questionnaires, including a peer-reviewed system usability scale and cybersickness evaluation. Descriptive statistics summarized participant traits and perceptions, with NVivo10 used for thematic analysis of qualitative feedback.
Results: Participants consisted mainly of women (64%), aged 30-39 (71%), with the majority being General Pediatrics residents (86%). Although 57% had no prior VR experience and none had used it clinically, most (71%) felt reasonably comfortable using it in practice. They found the VR clinic user-friendly, realistic, and conducive to trust and comfort (Table 1). Compared to face-to-face communication (F2F), 50% preferred VR, and 43% found it on par with F2F. The benefits of VR, as noted by participants, include potentially enhancing patient disclosure, comfort, and the doctor-patient relationship. Cybersickness symptoms experienced include slight discomfort, eye strain, and dizziness (Table 2). Those with prior VR exposure reported fewer symptoms compared to those who had never used VR (mean = 1.4 vs 3). The system's usability score was 73.9, indicating good usability.
Conclusion(s): Physicians responded favorably to VR technology, finding it easy to use and beneficial for doctor-patient relationships. Many preferred VR over F2F communication. The study suggests that VR could aid communication with adolescents in healthcare, potentially improving MH care by increasing disclosure and enhancing comfort for both patients and physicians. Future steps involve assessing VR's use in MH care from the patient's perspective and evaluating expansion in clinical settings.
.png)
.png)
