Nephrology
Session: Nephrology 4
25 - Patient and Caregiver Perspectives of Physical Activity Participation in Pediatric Chronic Kidney Disease
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 25
Publication Number: 25.1773
Publication Number: 25.1773
- AK
Amy Kogon, MD MPH
Assistant Professor of Pediatrics
CHOP
philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: Physical activity (PA) is critical to enhance health and quality of life, yet less than 15% of teens with chronic kidney disease (CKD) meet Department of Health and Human Services recommendations. PA mitigates cardiovascular disease, a leading cause of death for children with CKD. Identification of CKD-specific barriers and facilitators to PA is critical to develop effective interventions to promote PA as a therapy to improve outcomes.
Objective: To identify perspectives related to facilitators of and barriers to PA participation of teens with CKD and their caregivers.
Design/Methods: A study team of CKD and qualitative methods experts developed a semi-structured facilitation guide ascertaining mediators of patient participation in PA, exploring central domains including personal beliefs, the role of their environment, family, peers, and nephrologist’s attitudes. Interviews were conducted by telephone with teens (12-18 years old), and caregivers of teens, with CKD stages 2-5, not on kidney replacement therapy. The study team reviewed transcripts and used an integrated approach to develop a codebook, including conceptual, relationship, and participant perspective codes. Two coders used NVivo software to facilitate coding and memoing, using inter-rater reliability queries and full team discussions to ensure valid and reliable application of codes.
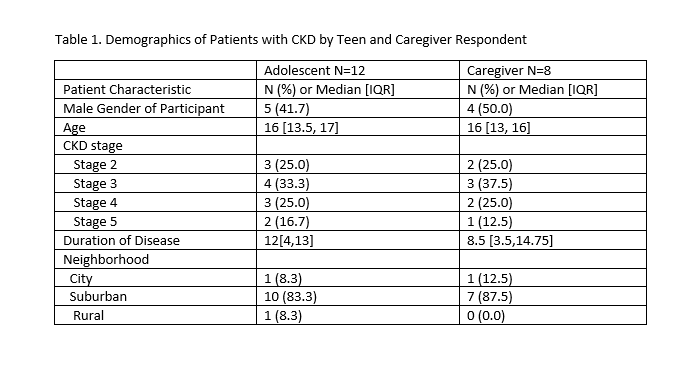
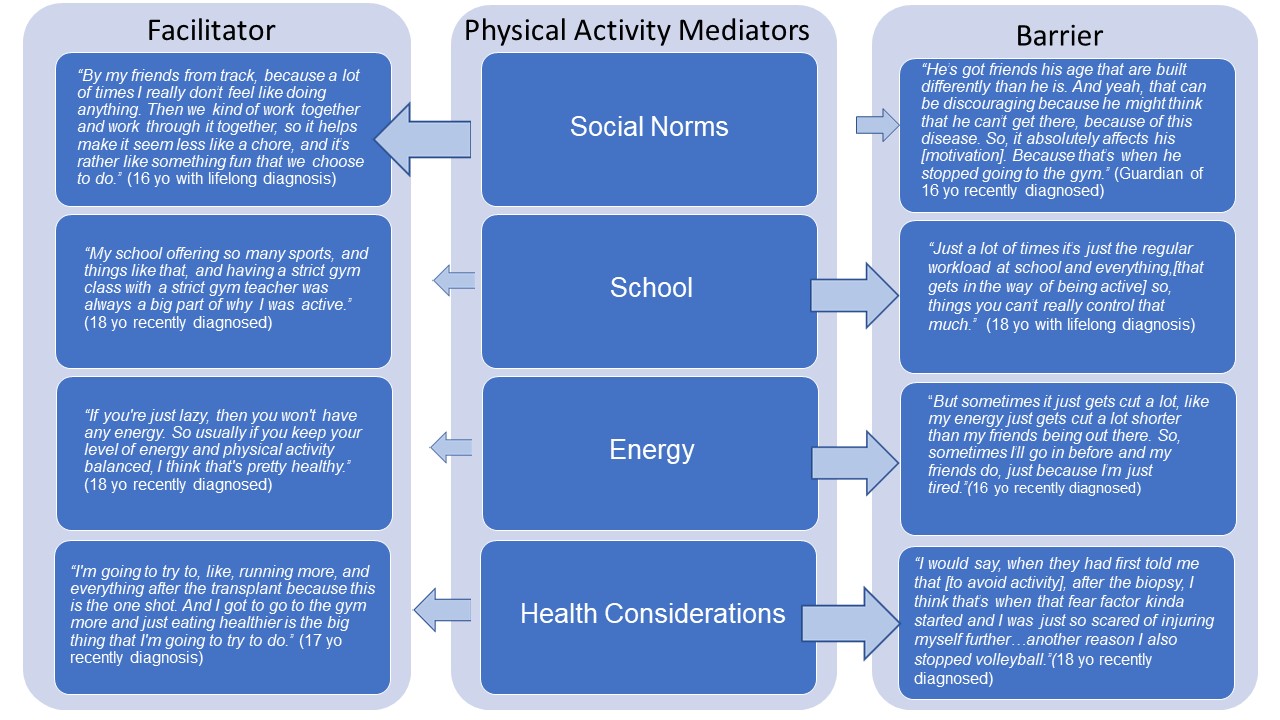
Results: Twelve teens and 8 caregivers participated (Table 1). Most were diagnosed at a young age. Participant and caregiver input were similar and clustered around key drivers of PA: social norms, energy, school, and health considerations. The most common facilitator was social norms. Participants described PA driven by sports teams and exercise with family or pets. A few felt discouraged from PA with concerns for not being able to keep up with peers. Primary barriers to PA were poor energy, especially after school, and the impact of school on time. Several teens described quitting sports because of kidney biopsies or future transplantation. One teen reported, “shutting down” his passions in response to progression of CKD. Many respondents denied discussing the benefits of PA with their nephrologists. Alternatively, they internalized messages concerning the health risks associated with PA, particularly contact sports and weightlifting. (Figure 1)
Conclusion(s): This study identified possible ways to promote PA in teens with CKD. Encouraging PA within a social setting can be a prime facilitator. Additionally, physicians can incorporate guidance that emphasizes the health benefits of PA and that strategizes how to safely engage in it without fear.