Child Abuse & Neglect
Session: Child Abuse & Neglect 2
194 - Variation in use of neuroimaging in the care of infants undergoing subspecialty evaluations for abuse: A multicenter study
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 194
Publication Number: 194.1588
Publication Number: 194.1588

Emily R. Alpert, BA (she/her/hers)
Medical Student
Perelman School of Medicine at the University of Pennsylvania
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: Well-appearing infants with concern for physical abuse are at risk for clinically occult intracranial injuries (ICI). Neuroimaging is necessary to identify these injuries, yet clear guidelines are not available. Identification of variation in neuroimaging use across hospitals and/or possible disparities would support guideline development.
Objective: Our objectives were: 1) quantify variation in neuroimaging use in the care of infants undergoing abuse evaluations without overt signs of ICI or blunt head injury and 2) assess for differences in neuroimaging use based on race/ethnicity and insurance type that could suggest disparities.
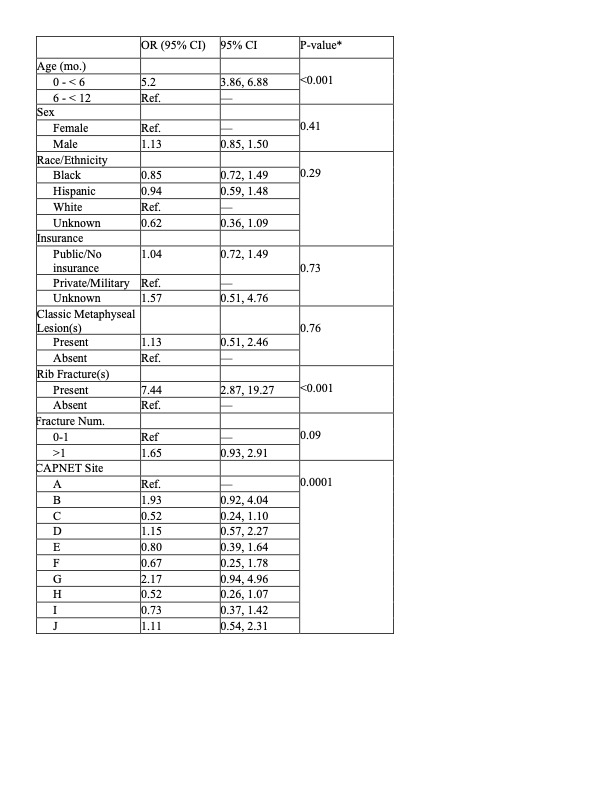
Design/Methods: Our sample included infants < 12 months receiving subspecialty child protection evaluation from 02/2021 – 05/2022 at 10 hospitals in CAPNET, a multicenter child abuse research network. Infants were included if they underwent a skeletal survey and lacked overt signs of possible ICI (e.g., seizures, altered mental status) or signs of blunt head injury (e.g., fracture, scalp swelling). Outcome was completion of neuroimaging (computed tomography (CT), standard magnetic resonance imaging (MRI), or fast MRI). We performed unadjusted tests of association (chi-square) of neuroimaging with age ( < 6 mo. vs 6- < 12 mo.), presence of a classic metaphyseal lesion (CML), rib fracture, >1 fracture, sex, race/ethnicity, insurance type, and CAPNET site. We performed multivariable logistic regression with all covariates. We then performed marginal standardization to calculate the adjusted percentages of infants undergoing neuroimaging across sites.
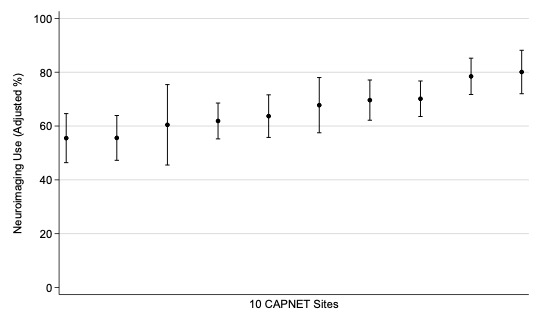
Results: Of 1119 infants, 745 (66.6%) underwent neuroimaging, with rates ranging from 51.0 to 80.2% across hospitals. In unadjusted analyses, there was an association between neuroimaging use and young age, presence of rib fractures, CMLs, multiple fractures, and CAPNET site (Table 1). In multivariable logistic regression, age, the presence of rib fractures, and CAPNET site remained significant (Table 2). In unadjusted and adjusted analyses, there was no association with race/ethnicity or insurance type. After adjustment for case-mix, there was significant variation (P < 0.001) across hospitals, with neuroimaging use ranging from 55.5% (95% CI: 46.4%, 64.6%) to 80.1% (95% CI 72.0, 88.1%) (Figure).
Conclusion(s): There was no evidence of disparities based on race/ethnicity or insurance type. We identified significant variation in neuroimaging use across hospitals, highlighting the need for guidelines and care standardization of neuroimaging for infants with concern for abuse.
.jpg)